
Contributions
Abstract: EP993
Type: E-Poster Presentation
Session title: Myeloma and other monoclonal gammopathies - Clinical
Background
Dyspnea in patients with AL amyloidosis is a common symptom usually attributed to cardiac dysfunction. Lung involvement is not a common feature of the disease and requires histopathological verification and a symptomatic presentation or typical radiographic changes of diffuse interstitial lung disease. However, post-mortem data and some retrospective studies suggest that lung involvement is likely underrecognized. A systematic functional approach of lung function in these patients is lacking.
Aims
To perform a comprehensive evaluation of lung function in consecutive patients with newly diagnosed AL amyloidosis.
Methods
This non-interventional, prospective study included 139 consecutive patients with systemic AL amyloidosis treated in the Department of Clinical Therapeutics (Athens, Greece). Patients with localized lung amyloidosis were excluded. Pulmonary function tests (PFTs) were performed in a Master screen Body (Jaeger, Germany). Spirometry, lung volume measurements, carbon monoxide diffusion capacity (DLCO) corrected for hemoglobin, maximal expiratory (Pe) and inspiratory (Pi) pressures were measured in a sitting position. Patient’s age, height and weight were recorded for use in the calculation of reference values.
Results
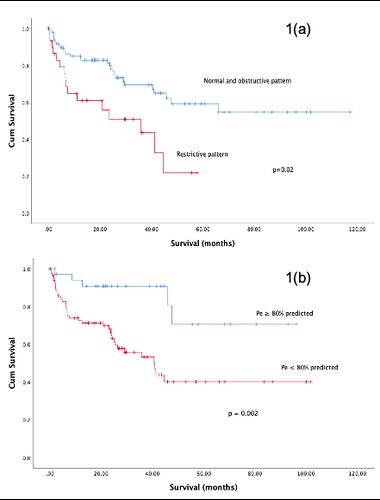
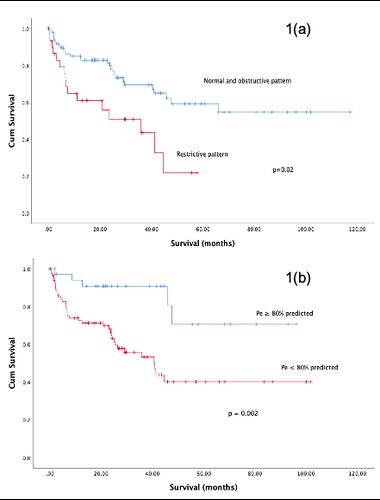
Median age was 65 years, 59% of patients were male; 65% had renal, 79% cardiac, 24% liver, 22% peripheral/autonomic and 2% lung involvement. Mayo stage distribution was as follows; 10% stage I, 52% stage II, 31% stage IIIa and 7% stage IIIb. Among patients, 68% had a normal breathing pattern, 9% obstructive and 23% restrictive. A restrictive pattern was associated with advanced Mayo stage (p=0.034); there was no association with free light chain (FLC) levels. One-year mortality for patients with a normal pattern was 14% versus 18% with obstructive and 38% for patients with a restrictive pattern. In univariate analysis, a restrictive breathing pattern was associated with worse survival (28.6 vs 76 months for patients with obstructive/normal pattern, p=0.002) and remained significant even after adjustment for Mayo stage (HR: 2.01, p=0.034). Certain indices of PFTs which reflect neuromuscular fitness and not breathing pattern (Pi and Pe), were severely affected in the majority of patients (93% for Pi and 61% for Pe had <80% of predicted values). Among PFT indices, FEV%, FVC1%, TLC, DLCO and Pe% were all associated with survival. Importantly, each of FEV1%<80%, FVC1%<80% and Pe% <80% of predicted remained significant for survival when adjusted individually for Mayo stage (FEV1%<80%, HR:2.1, p=0.016, FVC1%<80% HR:2.8, p<0.001, Pe% <80%, HR: 4.6, p=0.002). Low Pe% remained an independent prognostic factor for survival (HR 3.1, p=0.005) even when adjusted for the breathing pattern (restrictive versus normal/obstructive). Furthermore, among patients with stage IIIb disease, a low Pe% could further identify and ultra-high risk subgroup with even worse outcome (p=0.033).
Conclusion
In this comprehensive evaluation of lung function by PFTs we found that a restrictive breathing pattern is common in patients with systemic AL amyloidosis. Importantly, indices of PFTs associated with neuromuscular function are severely affected in most patients and are associated with prognosis, independently of the degree of cardiac dysfunction. Our results point to the presence of unrecognized pulmonary dysfunction, despite the absence of typical imaging findings, with prognostic and potentially therapeutic implications.
Keyword(s): AL amyloidosis, Prognosis
Abstract: EP993
Type: E-Poster Presentation
Session title: Myeloma and other monoclonal gammopathies - Clinical
Background
Dyspnea in patients with AL amyloidosis is a common symptom usually attributed to cardiac dysfunction. Lung involvement is not a common feature of the disease and requires histopathological verification and a symptomatic presentation or typical radiographic changes of diffuse interstitial lung disease. However, post-mortem data and some retrospective studies suggest that lung involvement is likely underrecognized. A systematic functional approach of lung function in these patients is lacking.
Aims
To perform a comprehensive evaluation of lung function in consecutive patients with newly diagnosed AL amyloidosis.
Methods
This non-interventional, prospective study included 139 consecutive patients with systemic AL amyloidosis treated in the Department of Clinical Therapeutics (Athens, Greece). Patients with localized lung amyloidosis were excluded. Pulmonary function tests (PFTs) were performed in a Master screen Body (Jaeger, Germany). Spirometry, lung volume measurements, carbon monoxide diffusion capacity (DLCO) corrected for hemoglobin, maximal expiratory (Pe) and inspiratory (Pi) pressures were measured in a sitting position. Patient’s age, height and weight were recorded for use in the calculation of reference values.
Results
Median age was 65 years, 59% of patients were male; 65% had renal, 79% cardiac, 24% liver, 22% peripheral/autonomic and 2% lung involvement. Mayo stage distribution was as follows; 10% stage I, 52% stage II, 31% stage IIIa and 7% stage IIIb. Among patients, 68% had a normal breathing pattern, 9% obstructive and 23% restrictive. A restrictive pattern was associated with advanced Mayo stage (p=0.034); there was no association with free light chain (FLC) levels. One-year mortality for patients with a normal pattern was 14% versus 18% with obstructive and 38% for patients with a restrictive pattern. In univariate analysis, a restrictive breathing pattern was associated with worse survival (28.6 vs 76 months for patients with obstructive/normal pattern, p=0.002) and remained significant even after adjustment for Mayo stage (HR: 2.01, p=0.034). Certain indices of PFTs which reflect neuromuscular fitness and not breathing pattern (Pi and Pe), were severely affected in the majority of patients (93% for Pi and 61% for Pe had <80% of predicted values). Among PFT indices, FEV%, FVC1%, TLC, DLCO and Pe% were all associated with survival. Importantly, each of FEV1%<80%, FVC1%<80% and Pe% <80% of predicted remained significant for survival when adjusted individually for Mayo stage (FEV1%<80%, HR:2.1, p=0.016, FVC1%<80% HR:2.8, p<0.001, Pe% <80%, HR: 4.6, p=0.002). Low Pe% remained an independent prognostic factor for survival (HR 3.1, p=0.005) even when adjusted for the breathing pattern (restrictive versus normal/obstructive). Furthermore, among patients with stage IIIb disease, a low Pe% could further identify and ultra-high risk subgroup with even worse outcome (p=0.033).
Conclusion
In this comprehensive evaluation of lung function by PFTs we found that a restrictive breathing pattern is common in patients with systemic AL amyloidosis. Importantly, indices of PFTs associated with neuromuscular function are severely affected in most patients and are associated with prognosis, independently of the degree of cardiac dysfunction. Our results point to the presence of unrecognized pulmonary dysfunction, despite the absence of typical imaging findings, with prognostic and potentially therapeutic implications.
Keyword(s): AL amyloidosis, Prognosis


