
Contributions
Abstract: EP980
Type: E-Poster Presentation
Session title: Myeloma and other monoclonal gammopathies - Clinical
Background
A prespecified interim efficacy analysis of the Phase 3 IKEMA study (NCT03275285) demonstrated that isatuximab (Isa) plus carfilzomib (K) and dexamethasone (d) (Isa-Kd) significantly improved progression-free survival (PFS) compared with Kd in patients (pts) with relapsed multiple myeloma (RMM) (HR 0.531; 99% CI, 0.318–0.889; P=0.0007), with a clinically meaningful increase in minimal residual disease negativity (MRD-) (29.6% vs 13.0%) and complete response (CR) (39.7% vs 27.6%) rates, and a manageable safety profile.
Aims
This subgroup analysis of IKEMA examined efficacy and safety in pts aged <70 and ≥70 years.
Methods
Pts with 1–3 prior lines of therapy were randomized 3:2 to receive Isa-Kd (n=179) or Kd (n=123). The primary end point was PFS, as assessed by an independent response committee. We compared outcomes in pts <70 vs ≥70 years; division into different or additional age groups resulted in smaller sample sizes.
Results
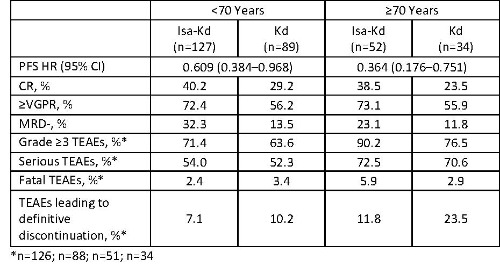
Of the 302 randomized pts, 71.5% were aged <70 years (Isa-Kd: 70.9%; Kd: 72.4%) and 28.5% were aged ≥70 years (Isa-Kd: 29.1%; Kd: 27.6%). Consistent with the significant improvement of PFS in the overall population, the addition of Isa to Kd resulted in improved PFS independently of age (Table). The CR, ≥very good partial response (VGPR), and MRD- rates were higher with Isa-Kd vs Kd. Within the Isa-Kd arm, CR rate and ≥VGPR rate were similar in elderly and younger pts. MRD- was observed in 32.3% of younger pts and 23.1% of elderly pts with Isa-Kd. In both arms, Grade ≥3 and serious treatment-emergent adverse events (TEAEs) were more frequently reported in elderly pts vs pts <70 years old (Table). For both age groups, the incidence of Grade ≥3 TEAEs was higher whereas the incidence of serious TEAEs was similar between Isa-Kd and Kd. In the elderly subgroup, 3 (5.9%) pts receiving Isa-Kd and 1 (2.9%) receiving Kd had fatal TEAEs (Isa-Kd, infection; Kd, general health deterioration due to progressive disease). The most common Grade ≥3 TEAEs in pts aged <70 and ≥70 years treated with Isa-Kd vs Kd were hypertension (18.3% vs 17.0% [<70 years] and 25.5% vs 26.5% [≥70 years]) and pneumonia (14.3% vs 9.1% [<70 years] and 21.6% vs 20.6% [≥70 years]).
Conclusion
The addition of Isa to Kd improved PFS and quality of response in elderly pts, with a manageable safety profile, consistent with the benefit observed in the overall IKEMA study population. Isa-Kd provides a potential new treatment option for elderly pts with RMM.
Keyword(s): Age, CD38, Multiple myeloma, Phase III
Abstract: EP980
Type: E-Poster Presentation
Session title: Myeloma and other monoclonal gammopathies - Clinical
Background
A prespecified interim efficacy analysis of the Phase 3 IKEMA study (NCT03275285) demonstrated that isatuximab (Isa) plus carfilzomib (K) and dexamethasone (d) (Isa-Kd) significantly improved progression-free survival (PFS) compared with Kd in patients (pts) with relapsed multiple myeloma (RMM) (HR 0.531; 99% CI, 0.318–0.889; P=0.0007), with a clinically meaningful increase in minimal residual disease negativity (MRD-) (29.6% vs 13.0%) and complete response (CR) (39.7% vs 27.6%) rates, and a manageable safety profile.
Aims
This subgroup analysis of IKEMA examined efficacy and safety in pts aged <70 and ≥70 years.
Methods
Pts with 1–3 prior lines of therapy were randomized 3:2 to receive Isa-Kd (n=179) or Kd (n=123). The primary end point was PFS, as assessed by an independent response committee. We compared outcomes in pts <70 vs ≥70 years; division into different or additional age groups resulted in smaller sample sizes.
Results
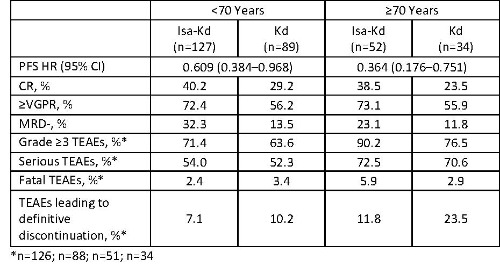
Of the 302 randomized pts, 71.5% were aged <70 years (Isa-Kd: 70.9%; Kd: 72.4%) and 28.5% were aged ≥70 years (Isa-Kd: 29.1%; Kd: 27.6%). Consistent with the significant improvement of PFS in the overall population, the addition of Isa to Kd resulted in improved PFS independently of age (Table). The CR, ≥very good partial response (VGPR), and MRD- rates were higher with Isa-Kd vs Kd. Within the Isa-Kd arm, CR rate and ≥VGPR rate were similar in elderly and younger pts. MRD- was observed in 32.3% of younger pts and 23.1% of elderly pts with Isa-Kd. In both arms, Grade ≥3 and serious treatment-emergent adverse events (TEAEs) were more frequently reported in elderly pts vs pts <70 years old (Table). For both age groups, the incidence of Grade ≥3 TEAEs was higher whereas the incidence of serious TEAEs was similar between Isa-Kd and Kd. In the elderly subgroup, 3 (5.9%) pts receiving Isa-Kd and 1 (2.9%) receiving Kd had fatal TEAEs (Isa-Kd, infection; Kd, general health deterioration due to progressive disease). The most common Grade ≥3 TEAEs in pts aged <70 and ≥70 years treated with Isa-Kd vs Kd were hypertension (18.3% vs 17.0% [<70 years] and 25.5% vs 26.5% [≥70 years]) and pneumonia (14.3% vs 9.1% [<70 years] and 21.6% vs 20.6% [≥70 years]).
Conclusion
The addition of Isa to Kd improved PFS and quality of response in elderly pts, with a manageable safety profile, consistent with the benefit observed in the overall IKEMA study population. Isa-Kd provides a potential new treatment option for elderly pts with RMM.
Keyword(s): Age, CD38, Multiple myeloma, Phase III


