
Contributions
Abstract: EP971
Type: E-Poster Presentation
Session title: Myeloma and other monoclonal gammopathies - Clinical
Background
Rapid induction of remission is a favorable prognostic factor in several cancers (Hodgkin’s and aggressive lymphomas). In multiple myeloma, only few data are available on response kinetics and outcome.
Aims
Here, we evaluated the association between time to best response in patients with transplant non-eligible, newly diagnosed multiple myeloma (TNE NDMM) enrolled in a randomized phase II study comparing KRd with KTd for induction and K with observation for maintenance therapy.
Methods
At time of data-cut (July 9, 2020), 91 patients were randomized and 80 patients with TNE NDMM received at least one cycle (=per protocol group) and have been analyzed so far in this still ongoing study. Median age was 75 years, ISS stage I/II/III: 21 (26.3%)/26 (32.5%)/33 (41.2%), ECOG stage 0/1: 40 (50%)/40 (50%). Patients were randomized for 9 cycles of KRd or KTd. After end of induction, those with SD or better were randomized to K maintenance (day 1 and 15) for 12 cycles or observation. MRD was assessed by NGF with a sensitivity of 10-6 in patients with ≥VGPR. To investigate whether time to best response influences survival, patients were assigned into quartiles. Response rates were evaluated by descriptive statistics, survival estimates calculated according to Kaplan-Meier and survival curves compared using the log-rank test. Fisher test was used for comparison of individual groups.
Results
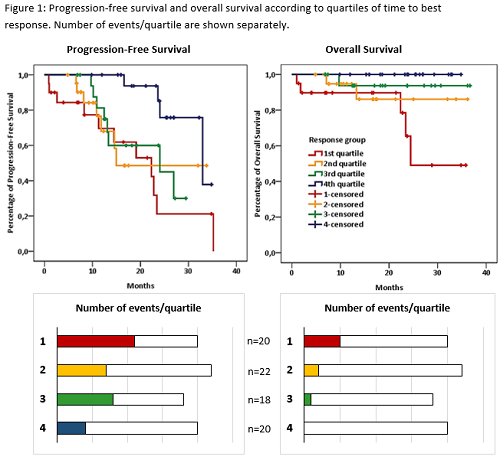
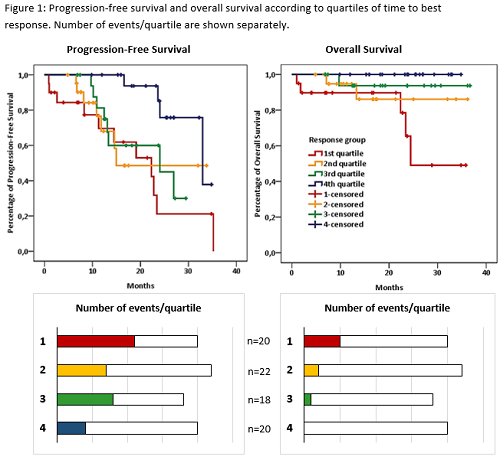
Median follow-up was 19.2 months. As the trial is still ongoing, response rates and survival data are given for both arms combined. Twenty-seven patients (33.8%) achieved CR, 33 patients (41.3%) VGPR, and 14 patients PR (17.5%). Six patients (7.5%) showed only minor or no response [MR: 3 (3.7%), SD: 2 (2.5%), PD: 1 (1.2%)]. Eleven patients discontinued therapy within the first cycle due to investigator decision [4 (4.4%)], patient’s decision [3 (3.3%)], development of AE/unacceptable toxicity [2 (2.2%)], and death or other reason [1 each (1.1%)], respectively. Eighteen of 40 patients (45%) tested were found to be MRD negative. The time to best response varied between 26 and 675 days. Quartile 1: 20 patients, days 26-42 days, quartile 2: 22 patients (43-112 days), quartile 3: 18 patients (113-253 days), quartile 4: 20 patients (254-675 days). The proportion of patients with progression or death declined from quartile 1 (55%) to quartile 2 (31.8%) and quartile 4 (20%). Only quartile 3 showed a rise up to 44.4% compared to quartile 2. Median progression-free survival was similar for patients of quartiles 1-3 (1: 22.3, 2: 15.0, 3: 24.0 months, p=0.645) but was significantly longer in those of quartile 4 (33.0 months, p=0.024, Fig. 1). Similar findings were observed for overall survival. There was a steady decrease in the proportion of death from quartile 1-4 (Fig. 1) and survival curves were similar for quartile 1-3 (p=0.143), but significantly superior for those of quartile 4 (p=0.019). Additional evaluations regarding high-risk cytogenetics, MRD negativity, depth of response or age did not reveal statistically significant differences, but showed tendencies that early responders include a higher proportion of patients with high-risk cytogenetics (presence of t(4;14) and/or del(17p)), MRD positivity and higher age. Updated results will be presented.
Conclusion
In conclusion, our data show that slow response kinetics are associated with prolonged progression-free and overall survival in patients randomized to either KRd or KTd induction therapy followed by one year of carfilzomib maintenance or observation.
Keyword(s): Imids, Multiple myeloma, Proteasome inhibitor
Abstract: EP971
Type: E-Poster Presentation
Session title: Myeloma and other monoclonal gammopathies - Clinical
Background
Rapid induction of remission is a favorable prognostic factor in several cancers (Hodgkin’s and aggressive lymphomas). In multiple myeloma, only few data are available on response kinetics and outcome.
Aims
Here, we evaluated the association between time to best response in patients with transplant non-eligible, newly diagnosed multiple myeloma (TNE NDMM) enrolled in a randomized phase II study comparing KRd with KTd for induction and K with observation for maintenance therapy.
Methods
At time of data-cut (July 9, 2020), 91 patients were randomized and 80 patients with TNE NDMM received at least one cycle (=per protocol group) and have been analyzed so far in this still ongoing study. Median age was 75 years, ISS stage I/II/III: 21 (26.3%)/26 (32.5%)/33 (41.2%), ECOG stage 0/1: 40 (50%)/40 (50%). Patients were randomized for 9 cycles of KRd or KTd. After end of induction, those with SD or better were randomized to K maintenance (day 1 and 15) for 12 cycles or observation. MRD was assessed by NGF with a sensitivity of 10-6 in patients with ≥VGPR. To investigate whether time to best response influences survival, patients were assigned into quartiles. Response rates were evaluated by descriptive statistics, survival estimates calculated according to Kaplan-Meier and survival curves compared using the log-rank test. Fisher test was used for comparison of individual groups.
Results
Median follow-up was 19.2 months. As the trial is still ongoing, response rates and survival data are given for both arms combined. Twenty-seven patients (33.8%) achieved CR, 33 patients (41.3%) VGPR, and 14 patients PR (17.5%). Six patients (7.5%) showed only minor or no response [MR: 3 (3.7%), SD: 2 (2.5%), PD: 1 (1.2%)]. Eleven patients discontinued therapy within the first cycle due to investigator decision [4 (4.4%)], patient’s decision [3 (3.3%)], development of AE/unacceptable toxicity [2 (2.2%)], and death or other reason [1 each (1.1%)], respectively. Eighteen of 40 patients (45%) tested were found to be MRD negative. The time to best response varied between 26 and 675 days. Quartile 1: 20 patients, days 26-42 days, quartile 2: 22 patients (43-112 days), quartile 3: 18 patients (113-253 days), quartile 4: 20 patients (254-675 days). The proportion of patients with progression or death declined from quartile 1 (55%) to quartile 2 (31.8%) and quartile 4 (20%). Only quartile 3 showed a rise up to 44.4% compared to quartile 2. Median progression-free survival was similar for patients of quartiles 1-3 (1: 22.3, 2: 15.0, 3: 24.0 months, p=0.645) but was significantly longer in those of quartile 4 (33.0 months, p=0.024, Fig. 1). Similar findings were observed for overall survival. There was a steady decrease in the proportion of death from quartile 1-4 (Fig. 1) and survival curves were similar for quartile 1-3 (p=0.143), but significantly superior for those of quartile 4 (p=0.019). Additional evaluations regarding high-risk cytogenetics, MRD negativity, depth of response or age did not reveal statistically significant differences, but showed tendencies that early responders include a higher proportion of patients with high-risk cytogenetics (presence of t(4;14) and/or del(17p)), MRD positivity and higher age. Updated results will be presented.
Conclusion
In conclusion, our data show that slow response kinetics are associated with prolonged progression-free and overall survival in patients randomized to either KRd or KTd induction therapy followed by one year of carfilzomib maintenance or observation.
Keyword(s): Imids, Multiple myeloma, Proteasome inhibitor


