Contributions
Abstract: EP934
Type: E-Poster Presentation
Session title: Myelodysplastic syndromes - Clinical
Background
MDS is a clonal blood stem cell disorder characterized by dysplasia and ineffective hematopoiesis leading to cytopenias and risk of transformation to AML. Post hoc analyses of a randomized phase 2 trial (NCT02610777) that compared pevonedistat + azacitidine (AZA) versus AZA alone, demonstrated that transformation to AML was associated with deterioration of quality of life (6/12 pts and 7/12 pts reported worsening of physical functioning and fatigue, respectively).1 Furthermore, OS was longer (median, 27.7 months [mths]) in pts who did not transform to AML [n=53] vs 13.6 mths in pts who did [n=14]; hazard ratio (HR), 0.289; p=0.0002).2
Aims
This retrospective study assessed the impact of AML transformation on OS in pts with HR-MDS receiving first-line therapy (1LT).
Methods
Pts with HR-MDS (≥18 years old) who initiated 1LT between Jan 1, 2008, and Jun 30, 2019, were identified from a large USA electronic medical record (EMR) database. Owing to lack of complete cytogenetics in the EMR, HR-MDS was defined based on International Classification of Diseases (ICD) coding for HR-MDS (≥1 ICD-9/-10 codes: 238.73, D46.2[0-2]) or an adapted HR-MDS algorithm based on the Revised International Prognostic Scoring System classification (intermediate or higher risk). Pts were followed from the start of HR-MDS 1LT until death, loss to follow-up or study end. Probability of transformation to AML following HR-MDS 1LT was assessed using Kaplan–Meier analysis. To account for differential follow-up time between pts who transformed to AML and pts who did not, a landmark analysis was conducted. The landmark time of 6 mths was chosen based on the guideline-recommended minimal duration of MDS treatment (6 cycles) and the median time to transformation (5.9 mths) among pts treated with AZA who transformed to AML (n=9/14) from the aforementioned study.2 In the landmark analysis, AML status (transformed to AML or not) was defined in the 6 mths following 1LT initiation in pts with ≥6 mths of follow-up. Cox proportional-hazards model was used to assess the impact of AML on OS from the landmark. To further validate the association between transformation to AML and OS, a time-varying Cox proportional-hazards model was considered, such that AML status was included as a time-varying variable. Both Cox models involved adjustments for baseline differences between pts with HR-MDS who transformed to AML and those who did not.
Results
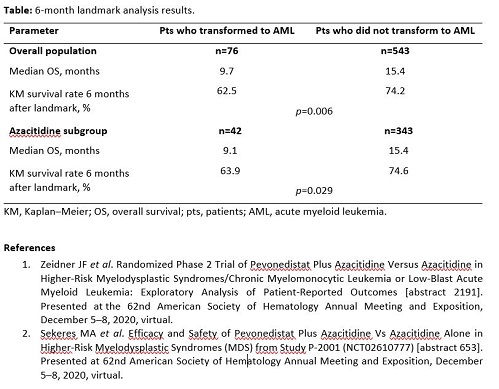
874 pts with HR-MDS were identified. Mean age was 71.9 years, and 43% had a Charlson comorbidity index of ≥2. Hypomethylating agents were the most common 1LT, with 62% of pts receiving AZA and 20% receiving decitabine. Median follow-up was 11.2 mths. In pts treated with 1LT, the rate of transformation to AML was 26.9% at 1 year and 39.4% at 2 years. The unadjusted landmark analysis showed shorter OS in pts who transformed to AML than in pts who did not (Table). These results were also consistent in subgroup of pts treated with AZA. Multivariable Cox proportional-hazard analysis also showed that transformation to AML was associated with worse survival. Pts who transformed to AML had a higher risk of death than pts who did not after adjusting for baseline differences in the 6-mth landmark analysis (HR, 1.82; 95% confidence interval [CI]: 1.18–2.81) and in the adjusted time-varying analysis at 1 year (HR, 2.85; 95% CI: 2.19–3.72).
Conclusion
Among treated pts with HR-MDS, transformation to AML was associated with inferior OS. These results highlight the importance of delaying transformation to AML as a treatment goal.
Keyword(s): MDS, MDS/AML, Survival, Transformation
Abstract: EP934
Type: E-Poster Presentation
Session title: Myelodysplastic syndromes - Clinical
Background
MDS is a clonal blood stem cell disorder characterized by dysplasia and ineffective hematopoiesis leading to cytopenias and risk of transformation to AML. Post hoc analyses of a randomized phase 2 trial (NCT02610777) that compared pevonedistat + azacitidine (AZA) versus AZA alone, demonstrated that transformation to AML was associated with deterioration of quality of life (6/12 pts and 7/12 pts reported worsening of physical functioning and fatigue, respectively).1 Furthermore, OS was longer (median, 27.7 months [mths]) in pts who did not transform to AML [n=53] vs 13.6 mths in pts who did [n=14]; hazard ratio (HR), 0.289; p=0.0002).2
Aims
This retrospective study assessed the impact of AML transformation on OS in pts with HR-MDS receiving first-line therapy (1LT).
Methods
Pts with HR-MDS (≥18 years old) who initiated 1LT between Jan 1, 2008, and Jun 30, 2019, were identified from a large USA electronic medical record (EMR) database. Owing to lack of complete cytogenetics in the EMR, HR-MDS was defined based on International Classification of Diseases (ICD) coding for HR-MDS (≥1 ICD-9/-10 codes: 238.73, D46.2[0-2]) or an adapted HR-MDS algorithm based on the Revised International Prognostic Scoring System classification (intermediate or higher risk). Pts were followed from the start of HR-MDS 1LT until death, loss to follow-up or study end. Probability of transformation to AML following HR-MDS 1LT was assessed using Kaplan–Meier analysis. To account for differential follow-up time between pts who transformed to AML and pts who did not, a landmark analysis was conducted. The landmark time of 6 mths was chosen based on the guideline-recommended minimal duration of MDS treatment (6 cycles) and the median time to transformation (5.9 mths) among pts treated with AZA who transformed to AML (n=9/14) from the aforementioned study.2 In the landmark analysis, AML status (transformed to AML or not) was defined in the 6 mths following 1LT initiation in pts with ≥6 mths of follow-up. Cox proportional-hazards model was used to assess the impact of AML on OS from the landmark. To further validate the association between transformation to AML and OS, a time-varying Cox proportional-hazards model was considered, such that AML status was included as a time-varying variable. Both Cox models involved adjustments for baseline differences between pts with HR-MDS who transformed to AML and those who did not.
Results
874 pts with HR-MDS were identified. Mean age was 71.9 years, and 43% had a Charlson comorbidity index of ≥2. Hypomethylating agents were the most common 1LT, with 62% of pts receiving AZA and 20% receiving decitabine. Median follow-up was 11.2 mths. In pts treated with 1LT, the rate of transformation to AML was 26.9% at 1 year and 39.4% at 2 years. The unadjusted landmark analysis showed shorter OS in pts who transformed to AML than in pts who did not (Table). These results were also consistent in subgroup of pts treated with AZA. Multivariable Cox proportional-hazard analysis also showed that transformation to AML was associated with worse survival. Pts who transformed to AML had a higher risk of death than pts who did not after adjusting for baseline differences in the 6-mth landmark analysis (HR, 1.82; 95% confidence interval [CI]: 1.18–2.81) and in the adjusted time-varying analysis at 1 year (HR, 2.85; 95% CI: 2.19–3.72).
Conclusion
Among treated pts with HR-MDS, transformation to AML was associated with inferior OS. These results highlight the importance of delaying transformation to AML as a treatment goal.
Keyword(s): MDS, MDS/AML, Survival, Transformation