
Contributions
Abstract: EP933
Type: E-Poster Presentation
Session title: Myelodysplastic syndromes - Clinical
Background
Myelodysplastic syndromes (MDS) are clonal hemopathies with a heterogeneous spectrum of presentation and a variable risk of transformation into acute myeloblastic leukemia (AML). Autoimmune diseases (AID) are present in 10 to 30% of cases, with unclear prognostic significance in this context. To date, the role of the R-IPSS in the context of an AID after an SMD has not yet been established.
Aims
To test the R-IPSS as a predictor as a predictor score of death/AML progression in MDS patients with AID. Secondary objectives were to study the association between the R-IPSS and the occurrence of an AID and the impact of AIDs on overall survival and leukemia-free survival (LFS).
Methods
We retrospectively collected data from primary MDS adult patients followed-up in the University Hospital of Poitiers between January 2010 and December 2019. Immunosuppressive therapy secondary-MDS were excluded. The date of onset and type of AID, as established by the standard criteria were collected. Simultaneous diagnoses of MDS and AID were considered if established in a 3-month interval from the MDS one. Left-censored patients (AID diagnosis before SMD) were dropped for the final survival analysis. A multistate cox model was performed with AID as an intermediate state. Baseline hazards proportionality for transitions to fatal events was tested by graph methods and checking the Schoenfeld residuals.
Results
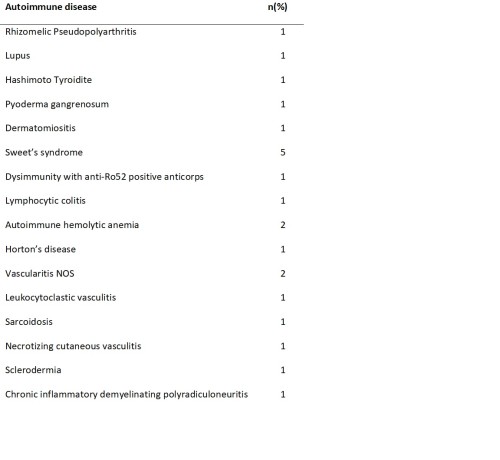
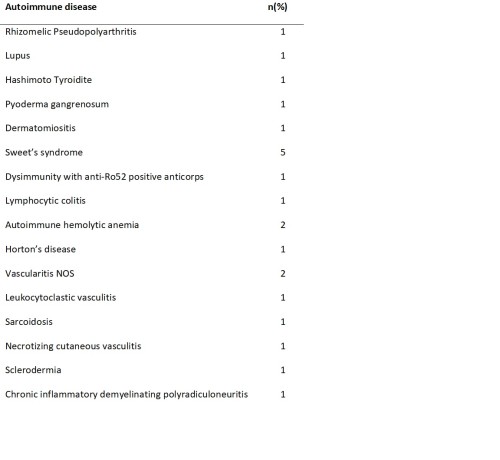
AIDs were identified in 22 of 212 MDS patients (10.4%). MDS-AID patients were equally sex-distributed (p=0.45). Associated AIDs were as specified in table 1. At the time of SMD diagnosis, 54.2% of patients had general signs and 13% had cutaneous and/or joint signs. No association between AID and WHO MDS-subtypes was observed. We found a trend-significant benefic effect of low-risk R-IPSS (<3.5 points) on the development of an AID (HR 0.44; 95%CI 0.2-1.2; p=0.1). In this setting, skin symptoms were the only associated factor in our cohort (HR 6.7; 95%CI 2.7-16.4; p<0.001). Fifteen of 22 MDS-AID patients suffered from death/AML progression. As expected, R-IPSS was a good predictor for the combined endpoint of death and AML progression in the whole MDS cohort. However, once patients develop an AID, R-IPSS did not associate with fatal events (HR 3.5; 95%CI 0.5-24.1; p=0.2). In this setting, only the presence of cutaneous and general symptoms were associated with death/AML.
Conclusion
The association of MDS to AIDs is of clinical heterogeneous expression. It tends to occur in low-risk MDS and does not seem to impact overall survival in our cohort.
The R-IPSS score (trend significantly) predicts the development of an AID (with an excess of risk for low-risk patients in our cohort) but once the autoimmune disease developed, it does not predicts accurately fatal events (AML and death). This finding lets us hypothesize the bigger role of AIDs severity than MDS factors in the mortality of MDS-AID.
Keyword(s): Autoimmune disease, Myelodysplasia
Abstract: EP933
Type: E-Poster Presentation
Session title: Myelodysplastic syndromes - Clinical
Background
Myelodysplastic syndromes (MDS) are clonal hemopathies with a heterogeneous spectrum of presentation and a variable risk of transformation into acute myeloblastic leukemia (AML). Autoimmune diseases (AID) are present in 10 to 30% of cases, with unclear prognostic significance in this context. To date, the role of the R-IPSS in the context of an AID after an SMD has not yet been established.
Aims
To test the R-IPSS as a predictor as a predictor score of death/AML progression in MDS patients with AID. Secondary objectives were to study the association between the R-IPSS and the occurrence of an AID and the impact of AIDs on overall survival and leukemia-free survival (LFS).
Methods
We retrospectively collected data from primary MDS adult patients followed-up in the University Hospital of Poitiers between January 2010 and December 2019. Immunosuppressive therapy secondary-MDS were excluded. The date of onset and type of AID, as established by the standard criteria were collected. Simultaneous diagnoses of MDS and AID were considered if established in a 3-month interval from the MDS one. Left-censored patients (AID diagnosis before SMD) were dropped for the final survival analysis. A multistate cox model was performed with AID as an intermediate state. Baseline hazards proportionality for transitions to fatal events was tested by graph methods and checking the Schoenfeld residuals.
Results
AIDs were identified in 22 of 212 MDS patients (10.4%). MDS-AID patients were equally sex-distributed (p=0.45). Associated AIDs were as specified in table 1. At the time of SMD diagnosis, 54.2% of patients had general signs and 13% had cutaneous and/or joint signs. No association between AID and WHO MDS-subtypes was observed. We found a trend-significant benefic effect of low-risk R-IPSS (<3.5 points) on the development of an AID (HR 0.44; 95%CI 0.2-1.2; p=0.1). In this setting, skin symptoms were the only associated factor in our cohort (HR 6.7; 95%CI 2.7-16.4; p<0.001). Fifteen of 22 MDS-AID patients suffered from death/AML progression. As expected, R-IPSS was a good predictor for the combined endpoint of death and AML progression in the whole MDS cohort. However, once patients develop an AID, R-IPSS did not associate with fatal events (HR 3.5; 95%CI 0.5-24.1; p=0.2). In this setting, only the presence of cutaneous and general symptoms were associated with death/AML.
Conclusion
The association of MDS to AIDs is of clinical heterogeneous expression. It tends to occur in low-risk MDS and does not seem to impact overall survival in our cohort.
The R-IPSS score (trend significantly) predicts the development of an AID (with an excess of risk for low-risk patients in our cohort) but once the autoimmune disease developed, it does not predicts accurately fatal events (AML and death). This finding lets us hypothesize the bigger role of AIDs severity than MDS factors in the mortality of MDS-AID.
Keyword(s): Autoimmune disease, Myelodysplasia


