
Contributions
Abstract: EP927
Type: E-Poster Presentation
Session title: Myelodysplastic syndromes - Clinical
Background
Myelofibrosis (MF) is observed in 10-20% of patients with myelodysplastic syndrome (MDS). The presence of MF≥2 according to the European Myelofibrosis Network (EUMNET 2005) has been recognized as an adverse histological finding associated with an aggressive course including early bone marrow failure, shortened survival and leukemic evolution. According to a previous survey performed by our group, the bone marrow biopsy is the most available complemental study in our media. Therefore improving the knowledge of variables related with MF and their prognostic role in patients with MDS is highly desirable.
Aims
To examine the influence of the presence of any degree of myelofibrosis (MF≥1) in overall survival (0S) in an Argentine MDS cohort and its association with clinical and histopathologic variables such as percentage of blasts, bone marrow cellularity, atypical erythroid localization and dysplastic megakaryocytes.
Methods
We identified 468 MDS patients from a multicentric retrospective database of 706 patients who were included in the Argentinian Registry of MDS from 2007 to 2017, with recorded evaluation of MF in the bone marrow biopsy. Statistical analysis included Kaplan-Meier and log rank test, Cox proportional hazard and Logistic regression.
Results
From the selected cohort, 32.7% had MF≥1, 25.8% (n=121) with MF-1, 5.7% (n=27) with MF-2 and 1% (n=5) had MF-3. When analyzing the characteristics of the population, we observe that the median age of these patients was 70 years old (Interquartile range 60-78) being 66.1% >65 years old and 55.8% were males. At the time of diagnosis we observe: median hemoglobin 9.0g/dL, platelet counts 121.500/mL and neutrophils 1.800/µL; 25.7% poor karyotypes and 26.7% IPSS-R>3.5.
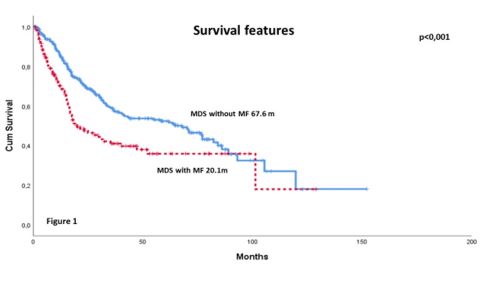
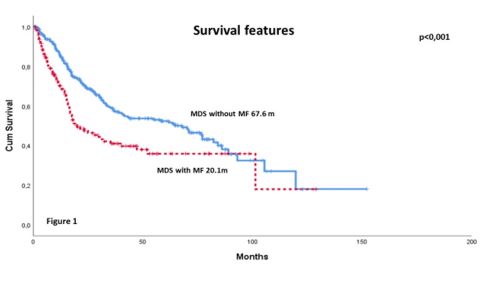
The median overall survival (OS) of the MF≥1 subgroup was 20.1 months (95% CI 10.1-30.0, p<0.001) versus MF-0 subgroup with 67.6 months (95%CI 45.1-90.3, p<0.001, Figure 1). Cox regression analysis revealed that MF≥1 (HR 1.46, 95% CI 1.06-2.03, p=0.020), performance status >2 (HR 2.07, 95% CI 1.44-2.96, p<0.001), hemoglobin level <10gr/dL (HR 1.64, 95% CI 1.16-2.32, p=0.005), platelet count <100.000/µL (HR 1.94, 95% CI 1.42-2.65, p<0.001), poor karyotypes (HR 1.86, 95% CI 1.32-2.63, p<0.001), bone marrow blasts ˃5% (HR 2.94, 95% CI 2.06-4.20, p<0.001) and Charlson Comorbidity Index >3 (HR 2.17, 95% CI 1.48-3.19, p<0.001) were independently associated with a reduced OS.
Regarding the association between MF≥1 and clinical and histopathologic features; this subgroup presented hemoglobin level <10gr/dL (p=0.003), ferritin level >1000mg/dL (p=0.004), increased bone marrow cellularity (p<0.001), atypical erythroid localization (p=0.002) and dysplastic megakaryocytes (p=0.006). Among these parameters, ferritin level (OR 3.41; p=0.006) and the atypical erythroid localization (0R 2.65; p=0.004) were significantly associated with the presence of MF≥1.
Conclusion
Our results highlight the presence of any grade of myelofibrosis in MDS as an independent adverse prognostic factor for survival in MDS. MF≥1 was also significantly associated with higher ferritin level and erythroid abnormalities in bone marrow.
Keyword(s): Bone Marrow Fibrosis, Myelodysplasia
Abstract: EP927
Type: E-Poster Presentation
Session title: Myelodysplastic syndromes - Clinical
Background
Myelofibrosis (MF) is observed in 10-20% of patients with myelodysplastic syndrome (MDS). The presence of MF≥2 according to the European Myelofibrosis Network (EUMNET 2005) has been recognized as an adverse histological finding associated with an aggressive course including early bone marrow failure, shortened survival and leukemic evolution. According to a previous survey performed by our group, the bone marrow biopsy is the most available complemental study in our media. Therefore improving the knowledge of variables related with MF and their prognostic role in patients with MDS is highly desirable.
Aims
To examine the influence of the presence of any degree of myelofibrosis (MF≥1) in overall survival (0S) in an Argentine MDS cohort and its association with clinical and histopathologic variables such as percentage of blasts, bone marrow cellularity, atypical erythroid localization and dysplastic megakaryocytes.
Methods
We identified 468 MDS patients from a multicentric retrospective database of 706 patients who were included in the Argentinian Registry of MDS from 2007 to 2017, with recorded evaluation of MF in the bone marrow biopsy. Statistical analysis included Kaplan-Meier and log rank test, Cox proportional hazard and Logistic regression.
Results
From the selected cohort, 32.7% had MF≥1, 25.8% (n=121) with MF-1, 5.7% (n=27) with MF-2 and 1% (n=5) had MF-3. When analyzing the characteristics of the population, we observe that the median age of these patients was 70 years old (Interquartile range 60-78) being 66.1% >65 years old and 55.8% were males. At the time of diagnosis we observe: median hemoglobin 9.0g/dL, platelet counts 121.500/mL and neutrophils 1.800/µL; 25.7% poor karyotypes and 26.7% IPSS-R>3.5.
The median overall survival (OS) of the MF≥1 subgroup was 20.1 months (95% CI 10.1-30.0, p<0.001) versus MF-0 subgroup with 67.6 months (95%CI 45.1-90.3, p<0.001, Figure 1). Cox regression analysis revealed that MF≥1 (HR 1.46, 95% CI 1.06-2.03, p=0.020), performance status >2 (HR 2.07, 95% CI 1.44-2.96, p<0.001), hemoglobin level <10gr/dL (HR 1.64, 95% CI 1.16-2.32, p=0.005), platelet count <100.000/µL (HR 1.94, 95% CI 1.42-2.65, p<0.001), poor karyotypes (HR 1.86, 95% CI 1.32-2.63, p<0.001), bone marrow blasts ˃5% (HR 2.94, 95% CI 2.06-4.20, p<0.001) and Charlson Comorbidity Index >3 (HR 2.17, 95% CI 1.48-3.19, p<0.001) were independently associated with a reduced OS.
Regarding the association between MF≥1 and clinical and histopathologic features; this subgroup presented hemoglobin level <10gr/dL (p=0.003), ferritin level >1000mg/dL (p=0.004), increased bone marrow cellularity (p<0.001), atypical erythroid localization (p=0.002) and dysplastic megakaryocytes (p=0.006). Among these parameters, ferritin level (OR 3.41; p=0.006) and the atypical erythroid localization (0R 2.65; p=0.004) were significantly associated with the presence of MF≥1.
Conclusion
Our results highlight the presence of any grade of myelofibrosis in MDS as an independent adverse prognostic factor for survival in MDS. MF≥1 was also significantly associated with higher ferritin level and erythroid abnormalities in bone marrow.
Keyword(s): Bone Marrow Fibrosis, Myelodysplasia


