
Contributions
Abstract: EP921
Type: E-Poster Presentation
Session title: Myelodysplastic syndromes - Clinical
Background
Low-risk myelodysplastic syndromes (LR-MDS) are a very heterogeneous group of diseases, ranging from mild forms, deserving follow-up only, to life-threatening cytopenias with frequent complications. There is growing interest on the immunologic proinflammatory bone marrow (BM) microenvironment of LR-MDS that may be of pathogenic but even of therapeutic relevance, since novel drugs targeting several cytokine patterns are under study.
Aims
To evaluate BM microenvironment of LR-MDS and its relationship with disease features, somatic mutations, and response to recombinant EPO (rEPO).
Methods
BM multiparameter flow cytometry (MFC) of patients with LR-MDS according to the revised international prognostic scoring system (IPSS-R) followed at a tertiary hematologic center have been retrospectively evaluated by 2 MFC experts. The proportions of the various lymphocyte populations (T, B, and NK cells), monocytes, and mastocytes have been evaluated using monoclonal antibodies directed against CD3, CD10, CD14, CD16, CD19, CD34, CD45, CD56, CD117, and HLA-DR.
Results
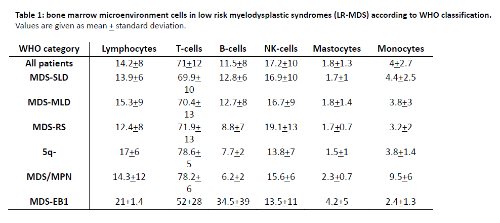
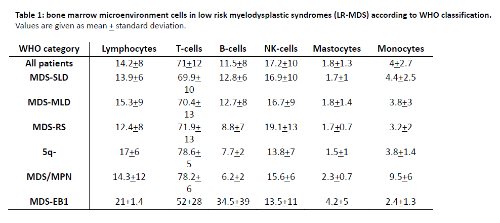
136 LR-MDS patients (48 multiple- and 38 single lineage dysplasia M-/SLD, 37 ring sideroblasts RS, 5 with 5q deletion, 5 MDS/myeloproliferative neoplasm overlap, and 2 excess of blasts type 1), 60% males and with a median age of 73.6 years (36-90.6), have been studied. Table 1 shows mean percentages of total lymphocytes, T-, B-, and NK-cells divided according to WHO type: MDS-RS showed significantly lower B cells and monocytes compared to patients with MDS-SLD (p=0.008 and p=0.03, respectively) and MDS-MLD (p=0.01 for B-cells). Elderly patients showed higher mastocyte levels (1.88+1.3% in >65 years vs 1.2+0.7% in younger patients, p=0.05). Concerning cytopenias, patients with Hb<10g/dL showed lower monocytes (3.4+2.2 vs 4.45+3%, p=0.02) compared to not anemic patients; those with PLT<100x10^9/L showed lower T-cells (67.2+15.4 vs 72.4+10.3%, p=0.02) and higher B-cells (14.2+11.5 vs 10.5+6.5%, p=0.02) compared to those with higher PLT; and subjects with neutrophils <1x10^9/L displayed higher mastocytes (2.5+2 vs 1.6+1%, p=0.004) and monocytes (5.5+4.08 vs 3.7+2.3%, p=0.004), as compared to those with higher values. Hypocellular patients showed increased total lymphocytes (20+9.3 vs 13+7.5%, p<0.0001) and NK-cells (21+17 vs 16.6+8%), and decreased mastocytes (1.2+1 vs 1.8+1.2%, p=0.03) compared to normo/hypercellular cases. Concerning somatic mutations, present in 27 out of 35 patients tested, the presence of >3 mutations was associated with increased total lymphocytes (22.4+14 vs 10.8+3.7%, p<0.001). Mutations of DNA methylation genes were related to lower T cells (69+11 vs 76+9%, p=0.04) and higher NK (18+8 vs 14+7%); mutated chromatin and transcription factor genes were associated with higher total lymphocytes (25+14 vs 11+6%, p=0.001 and 22.5+16.5 vs 12.3+6.8%, p=0.02, respectively). Mutations in TP53 or PHF6 were associated with increased T cells (83+0.7 vs 73+10%, p<0.001), mastocytes (2.4+1.4 vs 1.7+0.7, p<0.01), and monocytes (7.5+5 vs 3.8+2.3%, p=0.05), and decreased NK (7+1.4 vs 16+8, p<0.001). Regarding therapy, patients responding to rEPO showed reduced T cells (69+14 vs 76+10, p=0.05) and increased B cells (13+11 vs 7.5+5%, p=0.01).
Conclusion
Different types of LR-MDS show variable levels of BM lymphocyte, mastocyte and monocyte percentages. BM microenvironment characteristics correlate with cellularity and peculiar molecular alterations. Patients with greater T-cell infiltrate display higher frequency of disrupting mutations (i.e. TP53) and lower response to rEPO.
Keyword(s): Erythropoietin, Flow cytometry, Microenvironment, Myelodysplasia
Abstract: EP921
Type: E-Poster Presentation
Session title: Myelodysplastic syndromes - Clinical
Background
Low-risk myelodysplastic syndromes (LR-MDS) are a very heterogeneous group of diseases, ranging from mild forms, deserving follow-up only, to life-threatening cytopenias with frequent complications. There is growing interest on the immunologic proinflammatory bone marrow (BM) microenvironment of LR-MDS that may be of pathogenic but even of therapeutic relevance, since novel drugs targeting several cytokine patterns are under study.
Aims
To evaluate BM microenvironment of LR-MDS and its relationship with disease features, somatic mutations, and response to recombinant EPO (rEPO).
Methods
BM multiparameter flow cytometry (MFC) of patients with LR-MDS according to the revised international prognostic scoring system (IPSS-R) followed at a tertiary hematologic center have been retrospectively evaluated by 2 MFC experts. The proportions of the various lymphocyte populations (T, B, and NK cells), monocytes, and mastocytes have been evaluated using monoclonal antibodies directed against CD3, CD10, CD14, CD16, CD19, CD34, CD45, CD56, CD117, and HLA-DR.
Results
136 LR-MDS patients (48 multiple- and 38 single lineage dysplasia M-/SLD, 37 ring sideroblasts RS, 5 with 5q deletion, 5 MDS/myeloproliferative neoplasm overlap, and 2 excess of blasts type 1), 60% males and with a median age of 73.6 years (36-90.6), have been studied. Table 1 shows mean percentages of total lymphocytes, T-, B-, and NK-cells divided according to WHO type: MDS-RS showed significantly lower B cells and monocytes compared to patients with MDS-SLD (p=0.008 and p=0.03, respectively) and MDS-MLD (p=0.01 for B-cells). Elderly patients showed higher mastocyte levels (1.88+1.3% in >65 years vs 1.2+0.7% in younger patients, p=0.05). Concerning cytopenias, patients with Hb<10g/dL showed lower monocytes (3.4+2.2 vs 4.45+3%, p=0.02) compared to not anemic patients; those with PLT<100x10^9/L showed lower T-cells (67.2+15.4 vs 72.4+10.3%, p=0.02) and higher B-cells (14.2+11.5 vs 10.5+6.5%, p=0.02) compared to those with higher PLT; and subjects with neutrophils <1x10^9/L displayed higher mastocytes (2.5+2 vs 1.6+1%, p=0.004) and monocytes (5.5+4.08 vs 3.7+2.3%, p=0.004), as compared to those with higher values. Hypocellular patients showed increased total lymphocytes (20+9.3 vs 13+7.5%, p<0.0001) and NK-cells (21+17 vs 16.6+8%), and decreased mastocytes (1.2+1 vs 1.8+1.2%, p=0.03) compared to normo/hypercellular cases. Concerning somatic mutations, present in 27 out of 35 patients tested, the presence of >3 mutations was associated with increased total lymphocytes (22.4+14 vs 10.8+3.7%, p<0.001). Mutations of DNA methylation genes were related to lower T cells (69+11 vs 76+9%, p=0.04) and higher NK (18+8 vs 14+7%); mutated chromatin and transcription factor genes were associated with higher total lymphocytes (25+14 vs 11+6%, p=0.001 and 22.5+16.5 vs 12.3+6.8%, p=0.02, respectively). Mutations in TP53 or PHF6 were associated with increased T cells (83+0.7 vs 73+10%, p<0.001), mastocytes (2.4+1.4 vs 1.7+0.7, p<0.01), and monocytes (7.5+5 vs 3.8+2.3%, p=0.05), and decreased NK (7+1.4 vs 16+8, p<0.001). Regarding therapy, patients responding to rEPO showed reduced T cells (69+14 vs 76+10, p=0.05) and increased B cells (13+11 vs 7.5+5%, p=0.01).
Conclusion
Different types of LR-MDS show variable levels of BM lymphocyte, mastocyte and monocyte percentages. BM microenvironment characteristics correlate with cellularity and peculiar molecular alterations. Patients with greater T-cell infiltrate display higher frequency of disrupting mutations (i.e. TP53) and lower response to rEPO.
Keyword(s): Erythropoietin, Flow cytometry, Microenvironment, Myelodysplasia


