
Contributions
Abstract: EP912
Type: E-Poster Presentation
Session title: Myelodysplastic syndromes - Clinical
Background
MDS patients with a history of chemotherapy and/or radiation therapy for a malignant or non-malignant disease are considered to have therapy-related MDS (t-MDS). This group is generally described to constitute 15-20% of all MDS cases and to have more adverse prognostic factors such as transfusion dependency and high risk cytogenetics. They also have shorter survival and are often treated aggressively if possible. For t-MDS patients only treated with radiation, the data is conflicting
Aims
The aims of this study were to characterize t-MDS in a population-based setting, to compare clinical characteristics and outcomes between t-MDS and de novo MDS (d-MDS), and between subgroups of t-MDS.
Methods
All patients aged 16 years or older diagnosed with MDS and MDS/MPN 2009-2017 and reported to the nationwide Swedish MDS-register were included (n= 3379). All patients treated with chemotherapy and/or radiation prior to the diagnosis of MDS were considered to have t-MDS.
Data on previous cancer diagnoses was obtained from the Swedish Cancer Registry and data on non-malignant diseases from the National Patient Register. In cases with multiple malignant diseases preceding MDS, the most likely one was chosen based on latency time and treatment traditions. Information was obtained from the Swedish Cause of Death Register up to November 20, 2019 to calculate overall survival (OS).
To assess the distribution of baseline patient characteristics, chi-squared test and Wilcoxon rank sum test was used. OS was analysed using the Kaplan–Meier approach with log-rank test used to compare OS.
Results
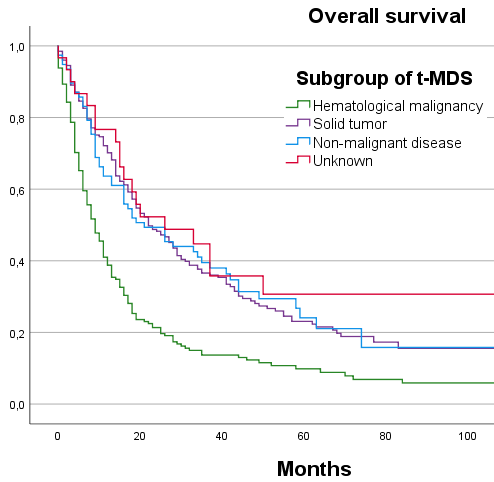
The median survival of the 14% (n=486) of patients classified as t-MDS was shorter compared to d-MDS, 16 vs 28 months (p=0.000). As a group, patients with t-MDS had more high risk cytogenetics, more transfusion dependency and a higher IPSS-R score compared to d-MDS. Patients previously treated with both chemotherapy and radiation and chemotherapy alone had a shorter median survival as compared to those treated with radiation only, 10 and 14 vs 32 months, respectively (p=0.000). Patients with a previous non-malignant disease or a previous solid tumour had a longer survival compared to patients with a previous hematological malignancy, 21 and 22 vs 9 months, respectively (p=0.000). To have the primary malignancy as an underlying cause of death was more common in patients with a previous hematological malignancy (43%) compared to patients with a previous solid malignancy (17%).
In the group of t-MDS patients previously treated with radiation only, known prognostic factors such as IPSS-R score, cytogenetics and transfusion dependency had a significantly lower risk profile compared to other groups of t-MDS. The most common primary condition in the group treated with radiation only was prostate cancer (41%) and breast cancer (20%).
Conclusion
Using Swedish register data we have characterized a large cohort of t-MDS. These patients have a significantly shorter survival as compared to d-MDS, but the survival difference is highly heterogeneous among subgroups. Patients previously treated with radiation only, have clinical characteristics and survival comparable to d-MDS and we question if these should be considered t-MDS. Patients with a previous hematological malignancy have a dismal prognosis, in part because of mortality associated with the primary condition.
Keyword(s): Epidemiology, MDS, Radiation
Abstract: EP912
Type: E-Poster Presentation
Session title: Myelodysplastic syndromes - Clinical
Background
MDS patients with a history of chemotherapy and/or radiation therapy for a malignant or non-malignant disease are considered to have therapy-related MDS (t-MDS). This group is generally described to constitute 15-20% of all MDS cases and to have more adverse prognostic factors such as transfusion dependency and high risk cytogenetics. They also have shorter survival and are often treated aggressively if possible. For t-MDS patients only treated with radiation, the data is conflicting
Aims
The aims of this study were to characterize t-MDS in a population-based setting, to compare clinical characteristics and outcomes between t-MDS and de novo MDS (d-MDS), and between subgroups of t-MDS.
Methods
All patients aged 16 years or older diagnosed with MDS and MDS/MPN 2009-2017 and reported to the nationwide Swedish MDS-register were included (n= 3379). All patients treated with chemotherapy and/or radiation prior to the diagnosis of MDS were considered to have t-MDS.
Data on previous cancer diagnoses was obtained from the Swedish Cancer Registry and data on non-malignant diseases from the National Patient Register. In cases with multiple malignant diseases preceding MDS, the most likely one was chosen based on latency time and treatment traditions. Information was obtained from the Swedish Cause of Death Register up to November 20, 2019 to calculate overall survival (OS).
To assess the distribution of baseline patient characteristics, chi-squared test and Wilcoxon rank sum test was used. OS was analysed using the Kaplan–Meier approach with log-rank test used to compare OS.
Results
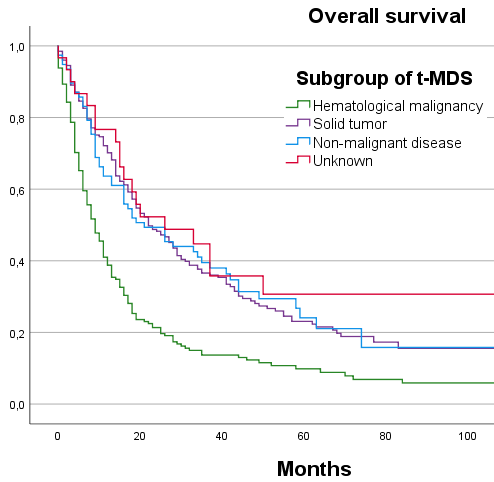
The median survival of the 14% (n=486) of patients classified as t-MDS was shorter compared to d-MDS, 16 vs 28 months (p=0.000). As a group, patients with t-MDS had more high risk cytogenetics, more transfusion dependency and a higher IPSS-R score compared to d-MDS. Patients previously treated with both chemotherapy and radiation and chemotherapy alone had a shorter median survival as compared to those treated with radiation only, 10 and 14 vs 32 months, respectively (p=0.000). Patients with a previous non-malignant disease or a previous solid tumour had a longer survival compared to patients with a previous hematological malignancy, 21 and 22 vs 9 months, respectively (p=0.000). To have the primary malignancy as an underlying cause of death was more common in patients with a previous hematological malignancy (43%) compared to patients with a previous solid malignancy (17%).
In the group of t-MDS patients previously treated with radiation only, known prognostic factors such as IPSS-R score, cytogenetics and transfusion dependency had a significantly lower risk profile compared to other groups of t-MDS. The most common primary condition in the group treated with radiation only was prostate cancer (41%) and breast cancer (20%).
Conclusion
Using Swedish register data we have characterized a large cohort of t-MDS. These patients have a significantly shorter survival as compared to d-MDS, but the survival difference is highly heterogeneous among subgroups. Patients previously treated with radiation only, have clinical characteristics and survival comparable to d-MDS and we question if these should be considered t-MDS. Patients with a previous hematological malignancy have a dismal prognosis, in part because of mortality associated with the primary condition.
Keyword(s): Epidemiology, MDS, Radiation


