
Contributions
Abstract: EP907
Type: E-Poster Presentation
Session title: Myelodysplastic syndromes - Biology & Translational Research
Background
Mesenchymal stromal cells (MSC) play a key role in the pathophysiology of MDS. Thus, MSC in MDS patients are abnormal and characterised by poor hematopoietic support capacity and their dysfunction contributes to the expansion of the malignant clone.
Aims
Considering the involvement of MSC in the pathophysiology of MDS, we aimed to study whether healthy MSC might have therapeutic potential in the positive regulation of residual healthy hematopoiesis in low-risk MDS patients.
Methods
Bone marrow (BM) samples from MDS patients (n=21), all from the low-risk MDS-DM category [WHO 2017] (IPSS: low/int-1 risk and IPSS-R: very low to intermediate) of new diagnosis and not exposed to haematological treatment, as well as from healthy donors (HD) (n=13), were analysed. Mononuclear cells (MNC) and MSC were isolated and expanded according to standard methodology up to 3rd-4th pass.
A short-term co-culture model was established in transwell (MNC:MSC ratio of 3:1, for 48h) with different cell combinations:
- Control MDS-MNC (basal MNC, not co-cultured).
- Control HD-MNC (basal MNC, not co-cultured)
- Group 1.1 - MDS-MSC co-cultured MDS-MNC
- Group 1.2 - MDS-MSC co-cultured HD-MNC
- Group 2.1 - HD-MSC co-cultured MDS-MNC
- Group 2.2 - HD-MSC co-cultured HD-MNC
- Group 3 - MDS-MSC co-cultured Mix-MNC (MDS+HD)
- Group 4 - HD-MSC co-cultured Mix-MNC (MDS+HD)
After 48h of culture, MNC from each group were collected and clonogenic assays were performed, from 5000 MNC seeded on semi-solid methylcellulose medium with EPO, at 37°C and 5% CO2. After 14 days of incubation, CFU-erythroid (CFU-E) and CFU-granulomonocytic (CFU-GM) were counted (CFU/5000 MNC).
Results
In basal state (without co-culture with MSC) MDS-MNC showed a deficient formation of CFU-E and CFU-GM compared to HD-MNC, as well as an imbalance between the number of CFU and clusters, which translates into defective hematopoiesis in MDS patients (not shown).
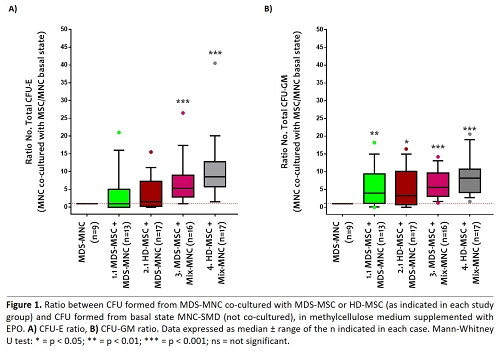
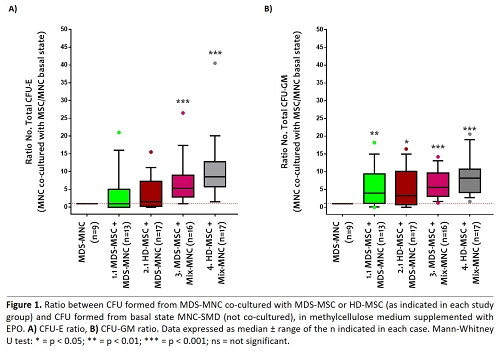
To determine the effect of the addition of MSC on MNC of MDS patients (groups 1.1 and 2.1), we analysed the ratio between CFU formed by MDS-MNC co-cultured with MSC (MDS or HD) versus basal MDS-MNC (not co-cultured). We observed that the addition of HD-MSC trends to increase erythroid colony formation (Fig. 1-A) and that CFU-granulomonocytic were significantly enhanced by addition of MSC (Fig. 1-B).
In an environment simulating the diseased condition (groups 3 and 4), with mixed MDS and HD MNC (residual hematopoiesis), a significant recovery of hematopoietic capacity occurs with the addition of MSC, greater if HD-MSC (Fig. 1, A and B).
Conclusion
Taken together, our results suggest that HD-MSC enhances MNC clonogenic capacity, especially when co-cultured with mixed MDS and HD MNC. Considering that this situation mimics what happens in lower-risk MDS patients, where often normal and dysplastic hemopoiesis coexists, HD-MSC could be a potential therapy to rescue residual healthy hematopoiesis and improve hematopoietic potential in these patients.
Keyword(s): Hematopoiesis, MDS, Mesenchymal stem cell
Abstract: EP907
Type: E-Poster Presentation
Session title: Myelodysplastic syndromes - Biology & Translational Research
Background
Mesenchymal stromal cells (MSC) play a key role in the pathophysiology of MDS. Thus, MSC in MDS patients are abnormal and characterised by poor hematopoietic support capacity and their dysfunction contributes to the expansion of the malignant clone.
Aims
Considering the involvement of MSC in the pathophysiology of MDS, we aimed to study whether healthy MSC might have therapeutic potential in the positive regulation of residual healthy hematopoiesis in low-risk MDS patients.
Methods
Bone marrow (BM) samples from MDS patients (n=21), all from the low-risk MDS-DM category [WHO 2017] (IPSS: low/int-1 risk and IPSS-R: very low to intermediate) of new diagnosis and not exposed to haematological treatment, as well as from healthy donors (HD) (n=13), were analysed. Mononuclear cells (MNC) and MSC were isolated and expanded according to standard methodology up to 3rd-4th pass.
A short-term co-culture model was established in transwell (MNC:MSC ratio of 3:1, for 48h) with different cell combinations:
- Control MDS-MNC (basal MNC, not co-cultured).
- Control HD-MNC (basal MNC, not co-cultured)
- Group 1.1 - MDS-MSC co-cultured MDS-MNC
- Group 1.2 - MDS-MSC co-cultured HD-MNC
- Group 2.1 - HD-MSC co-cultured MDS-MNC
- Group 2.2 - HD-MSC co-cultured HD-MNC
- Group 3 - MDS-MSC co-cultured Mix-MNC (MDS+HD)
- Group 4 - HD-MSC co-cultured Mix-MNC (MDS+HD)
After 48h of culture, MNC from each group were collected and clonogenic assays were performed, from 5000 MNC seeded on semi-solid methylcellulose medium with EPO, at 37°C and 5% CO2. After 14 days of incubation, CFU-erythroid (CFU-E) and CFU-granulomonocytic (CFU-GM) were counted (CFU/5000 MNC).
Results
In basal state (without co-culture with MSC) MDS-MNC showed a deficient formation of CFU-E and CFU-GM compared to HD-MNC, as well as an imbalance between the number of CFU and clusters, which translates into defective hematopoiesis in MDS patients (not shown).
To determine the effect of the addition of MSC on MNC of MDS patients (groups 1.1 and 2.1), we analysed the ratio between CFU formed by MDS-MNC co-cultured with MSC (MDS or HD) versus basal MDS-MNC (not co-cultured). We observed that the addition of HD-MSC trends to increase erythroid colony formation (Fig. 1-A) and that CFU-granulomonocytic were significantly enhanced by addition of MSC (Fig. 1-B).
In an environment simulating the diseased condition (groups 3 and 4), with mixed MDS and HD MNC (residual hematopoiesis), a significant recovery of hematopoietic capacity occurs with the addition of MSC, greater if HD-MSC (Fig. 1, A and B).
Conclusion
Taken together, our results suggest that HD-MSC enhances MNC clonogenic capacity, especially when co-cultured with mixed MDS and HD MNC. Considering that this situation mimics what happens in lower-risk MDS patients, where often normal and dysplastic hemopoiesis coexists, HD-MSC could be a potential therapy to rescue residual healthy hematopoiesis and improve hematopoietic potential in these patients.
Keyword(s): Hematopoiesis, MDS, Mesenchymal stem cell


