
Contributions
Abstract: EP886
Type: E-Poster Presentation
Session title: Lymphoma Biology & Translational Research
Background
There are conflicting data how obesity might affect outcomes in patients with classical Hodgkin lymphoma (cHL). Computed tomography (CT) scans done at the time of cHL staging offer a unique opportunity to assess different body fat compartments and their potential prognostic associations without exposing these patients to additional unnecessary procedures.
Aims
We aimed to assess subcutaneous and visceral abdominal fat measurements in patients with cHL at the time of diagnosis and to investigate their clinical associations.
Methods
We retrospectively analyzed 82 newly diagnosed cHL patients from our center with available CT scans prior to receiving specific therapy and with available clinical data. Patients were treated with either ABVD or eBEACOPP chemotherapy regimens and subsequent radiotherapy per physicians’ decision. Perirenal fat was chosen as a measurement of visceral fat and its thickness was assessed as the largest and the smallest distance from kidney outline to the inner limit of abdominal wall at the transversal level of the renal vein. Subcutaneous fat thickness was assessed as the largest distance between the skin and outer limit of the muscular abdominal wall at the transversal level of the umbilicus.
Results
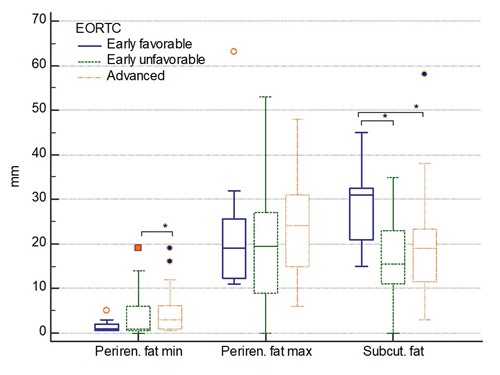
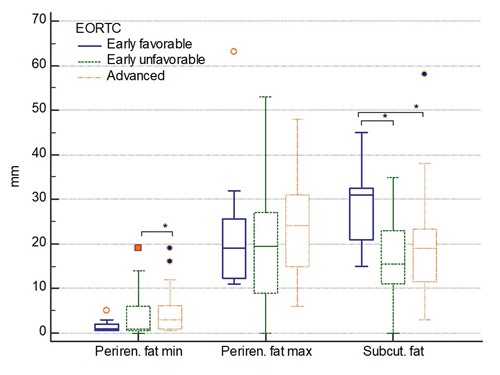
Median age was 36 years, majority of patients were males [46/82 (56.1%)]. The most common histological subtype was nodular sclerosis [61/82 (74.4%)]. A total of 11/82 (13.4%) patients were classified as early favorable, 38/82 (46.3%) as early unfavorable and 33/82 (40.2%) as advanced disease by EORTC system. All three abdominal fat thickness measurements (minimal and maximal perirenal and subcutaneous fat thickness) correlated positively together, showed moderate positive correlation with BMI (Rho 0.54 to 0.57; P<0.05) and weak positive correlation with total psoas muscle area at the L3 level (Rho 0.24 to 0.33; P<0.05).
Patients with more advanced EORTC disease stage were significantly more likely to have higher minimal perirenal fat thickness but lower subcutaneous fat thickness (P<0.05 for both analyses) as shown in Figure 1. Similarly, minimal perirenal fat thickness was significantly positively correlated with the IPS (Rho=0.34, P=0.002), whereas subcutaneous fat thickness was significantly negatively correlated with the IPS (Rho=-0.27, P=0.013). No significant associations of BMI with EORTC stages nor IPS were present (P>0.05).
Higher minimal (HR=8.4; P<0.001) and maximal perirenal fat thickness (HR=3.15; P=0.049), but lower subcutaneous fat thickness (HR=3.57; P=0.033) were associated with inferior overall survival in univariate analyses. In addition, lower subcutaneous fat thickness (HR=4.45; P=0.005) was also associated with shorter time to disease progression. There was no association of BMI with neither survival nor time to progression.
Associations of perirenal and subcutaneous fat thickness were further analyzed in the multivariate models adjusted for age, gender, Ann Arbor stage and IPS. Both minimal perirenal fat thickness >2 mm (HR=49.2; P=0.019), subcutaneous fat thickness ≤22 mm (HR=45.7; P=0.038) and IPS (HR=2.44; P=0.025) remained significantly associated with inferior overall survival. Subcutaneous fat ≤22 mm (HR=14.4; P=0.013) and older age (HR=1.04; P=0.043) remained independently associated with shorter time to disease progression.
Conclusion
Excess body fat might differently affect outcomes in patients with cHL depending on its distribution. Distinction between different abdominal adipose tissue compartments is necessary to better understand relationship between obesity, cachexia and prognosis in patients with cHL.
Keyword(s): Hodgkin's lymphoma, Obesity, Progression, Survival
Abstract: EP886
Type: E-Poster Presentation
Session title: Lymphoma Biology & Translational Research
Background
There are conflicting data how obesity might affect outcomes in patients with classical Hodgkin lymphoma (cHL). Computed tomography (CT) scans done at the time of cHL staging offer a unique opportunity to assess different body fat compartments and their potential prognostic associations without exposing these patients to additional unnecessary procedures.
Aims
We aimed to assess subcutaneous and visceral abdominal fat measurements in patients with cHL at the time of diagnosis and to investigate their clinical associations.
Methods
We retrospectively analyzed 82 newly diagnosed cHL patients from our center with available CT scans prior to receiving specific therapy and with available clinical data. Patients were treated with either ABVD or eBEACOPP chemotherapy regimens and subsequent radiotherapy per physicians’ decision. Perirenal fat was chosen as a measurement of visceral fat and its thickness was assessed as the largest and the smallest distance from kidney outline to the inner limit of abdominal wall at the transversal level of the renal vein. Subcutaneous fat thickness was assessed as the largest distance between the skin and outer limit of the muscular abdominal wall at the transversal level of the umbilicus.
Results
Median age was 36 years, majority of patients were males [46/82 (56.1%)]. The most common histological subtype was nodular sclerosis [61/82 (74.4%)]. A total of 11/82 (13.4%) patients were classified as early favorable, 38/82 (46.3%) as early unfavorable and 33/82 (40.2%) as advanced disease by EORTC system. All three abdominal fat thickness measurements (minimal and maximal perirenal and subcutaneous fat thickness) correlated positively together, showed moderate positive correlation with BMI (Rho 0.54 to 0.57; P<0.05) and weak positive correlation with total psoas muscle area at the L3 level (Rho 0.24 to 0.33; P<0.05).
Patients with more advanced EORTC disease stage were significantly more likely to have higher minimal perirenal fat thickness but lower subcutaneous fat thickness (P<0.05 for both analyses) as shown in Figure 1. Similarly, minimal perirenal fat thickness was significantly positively correlated with the IPS (Rho=0.34, P=0.002), whereas subcutaneous fat thickness was significantly negatively correlated with the IPS (Rho=-0.27, P=0.013). No significant associations of BMI with EORTC stages nor IPS were present (P>0.05).
Higher minimal (HR=8.4; P<0.001) and maximal perirenal fat thickness (HR=3.15; P=0.049), but lower subcutaneous fat thickness (HR=3.57; P=0.033) were associated with inferior overall survival in univariate analyses. In addition, lower subcutaneous fat thickness (HR=4.45; P=0.005) was also associated with shorter time to disease progression. There was no association of BMI with neither survival nor time to progression.
Associations of perirenal and subcutaneous fat thickness were further analyzed in the multivariate models adjusted for age, gender, Ann Arbor stage and IPS. Both minimal perirenal fat thickness >2 mm (HR=49.2; P=0.019), subcutaneous fat thickness ≤22 mm (HR=45.7; P=0.038) and IPS (HR=2.44; P=0.025) remained significantly associated with inferior overall survival. Subcutaneous fat ≤22 mm (HR=14.4; P=0.013) and older age (HR=1.04; P=0.043) remained independently associated with shorter time to disease progression.
Conclusion
Excess body fat might differently affect outcomes in patients with cHL depending on its distribution. Distinction between different abdominal adipose tissue compartments is necessary to better understand relationship between obesity, cachexia and prognosis in patients with cHL.
Keyword(s): Hodgkin's lymphoma, Obesity, Progression, Survival


