
Contributions
Abstract: EP832
Type: E-Poster Presentation
Session title: Infections in hematology (incl. supportive care/therapy)
Background
Patients with acute respiratory infection due to COVID 19 have an increased risk of thromboembolic disease. Coagulation activation, endothelial dysfunction, platelet activation and impaired fibrinolysis have all been proposed as directly involved in its pathogenesis. In Latin America, data regarding the incidence of acute thrombotic complications (venous and arterial) is scarce.
Aims
The aim of this analysis is to describe characteristics and outcomes of patients with confirmed COVID-19 infection with acute arterial and venous thrombotic events attended during a 10-month period, at a referral hospital in Mexico City.
Methods
We included consecutive critical and non-critical adult patients, hospitalized at Hospital Central Norte Pemex in Mexico City, between April 1, 2020 and January 31, 2021. All patients tested positive for SARS- CoV-2 using RT- PCR from nasopharyngeal and oropharyngeal swabs. Thrombotic events were diagnosed during clinical care. Thrombotic events included both venous (deep vein thrombosis [DVT]; pulmonary embolism [PE]) and arterial (myocardial infarction [MI], ischemic stroke, and other arterial thrombosis). All patients received thromboprophylaxis prior; and treatment (anticoagulation; platelet antiaggregation; a combination of both or other therapeutic interventions) at the time of diagnosis according to international and local recommendations.
Continuous variables (age, leucocyte count with differentials, hemoglobin, D-dimer, ferritin, LDH, etc.) are presented as mean ± standard deviation, (or median and range as appropriate) and were compared using the student-t or Mann-Whitney U test. All data were analyzed using SPSS version 21 statistics software. A p value <0.05 was considered statistically significant.
Results
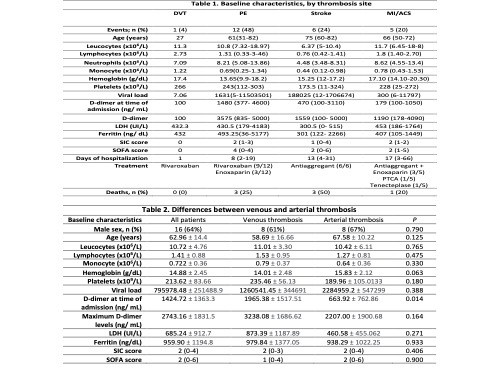
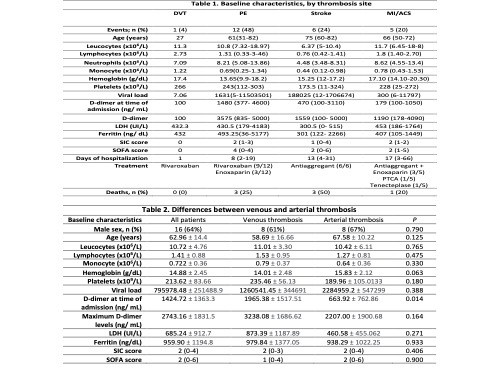
We analyzed 1379 hospitalized patients with confirmed COVID-19 infection. Twenty-five patients received a diagnosis of acute thrombotic events (1.81%): 13 cases (52%) of venous thrombosis (DVT: 1 case (4%); PE: 12 cases (48%)), and 12 cases (48%) of arterial thrombosis (acute Stroke: 6 cases (24%); MI/ACS: 5 cases (20%); and one case of Mesenteric thrombosis (4%)). Baseline characteristics are summarized in table 1. The mean age of all patients with thrombotic events was 62.96 14.4 years; and were predominantly male (64%).
Patients with venous thromboembolic events presented with higher D- dimer levels at the time of admission compared to those who had arterial thrombosis (mean 1965.38 vs 663.92, P= 0.014). We also observed a trend to higher hemoglobin levels at the time of diagnosis in patients with arterial events compared to cases of venous thromboembolism (mean 15.83 vs 14.01, P= 0.063). Comparison of patient’s characteristics between venous and arterial thrombosis is found in table 2.
The overall mortality of the group with thrombotic events was 28%. The main cause for death was respiratory failure due to acute respiratory distress syndrome (5 patients, 71%).
Conclusion
Our analysis shows a low venous thromboembolic rate compared with other groups, and similar to another series reported in our country. Interestingly, we observed a significant proportion of arterial thrombotic complications. However, this study has limitations. Venous thromboembolism may have been underdiagnosed because of limited imaging studies. Also, neurological or ischemic cardiac symptoms may have been underestimated in patients with severe COVID-19 infection. Changes in prophylactic anticoagulation strategies, as well as in clinical practice, could affect the incidence of thrombotic events.
Keyword(s): COVID-19, Thrombosis
Abstract: EP832
Type: E-Poster Presentation
Session title: Infections in hematology (incl. supportive care/therapy)
Background
Patients with acute respiratory infection due to COVID 19 have an increased risk of thromboembolic disease. Coagulation activation, endothelial dysfunction, platelet activation and impaired fibrinolysis have all been proposed as directly involved in its pathogenesis. In Latin America, data regarding the incidence of acute thrombotic complications (venous and arterial) is scarce.
Aims
The aim of this analysis is to describe characteristics and outcomes of patients with confirmed COVID-19 infection with acute arterial and venous thrombotic events attended during a 10-month period, at a referral hospital in Mexico City.
Methods
We included consecutive critical and non-critical adult patients, hospitalized at Hospital Central Norte Pemex in Mexico City, between April 1, 2020 and January 31, 2021. All patients tested positive for SARS- CoV-2 using RT- PCR from nasopharyngeal and oropharyngeal swabs. Thrombotic events were diagnosed during clinical care. Thrombotic events included both venous (deep vein thrombosis [DVT]; pulmonary embolism [PE]) and arterial (myocardial infarction [MI], ischemic stroke, and other arterial thrombosis). All patients received thromboprophylaxis prior; and treatment (anticoagulation; platelet antiaggregation; a combination of both or other therapeutic interventions) at the time of diagnosis according to international and local recommendations.
Continuous variables (age, leucocyte count with differentials, hemoglobin, D-dimer, ferritin, LDH, etc.) are presented as mean ± standard deviation, (or median and range as appropriate) and were compared using the student-t or Mann-Whitney U test. All data were analyzed using SPSS version 21 statistics software. A p value <0.05 was considered statistically significant.
Results
We analyzed 1379 hospitalized patients with confirmed COVID-19 infection. Twenty-five patients received a diagnosis of acute thrombotic events (1.81%): 13 cases (52%) of venous thrombosis (DVT: 1 case (4%); PE: 12 cases (48%)), and 12 cases (48%) of arterial thrombosis (acute Stroke: 6 cases (24%); MI/ACS: 5 cases (20%); and one case of Mesenteric thrombosis (4%)). Baseline characteristics are summarized in table 1. The mean age of all patients with thrombotic events was 62.96 14.4 years; and were predominantly male (64%).
Patients with venous thromboembolic events presented with higher D- dimer levels at the time of admission compared to those who had arterial thrombosis (mean 1965.38 vs 663.92, P= 0.014). We also observed a trend to higher hemoglobin levels at the time of diagnosis in patients with arterial events compared to cases of venous thromboembolism (mean 15.83 vs 14.01, P= 0.063). Comparison of patient’s characteristics between venous and arterial thrombosis is found in table 2.
The overall mortality of the group with thrombotic events was 28%. The main cause for death was respiratory failure due to acute respiratory distress syndrome (5 patients, 71%).
Conclusion
Our analysis shows a low venous thromboembolic rate compared with other groups, and similar to another series reported in our country. Interestingly, we observed a significant proportion of arterial thrombotic complications. However, this study has limitations. Venous thromboembolism may have been underdiagnosed because of limited imaging studies. Also, neurological or ischemic cardiac symptoms may have been underestimated in patients with severe COVID-19 infection. Changes in prophylactic anticoagulation strategies, as well as in clinical practice, could affect the incidence of thrombotic events.
Keyword(s): COVID-19, Thrombosis


