
Contributions
Abstract: EP826
Type: E-Poster Presentation
Session title: Infections in hematology (incl. supportive care/therapy)
Background
Reports on outcomes of COVID-19 in hematologic patients vary.
Aims
To describe outcomes and risk factors of SARS-CoV2 infection in patients treated in a large university medical center.
Methods
We analyzed the outcomes of our patients diagnosed with COVID-19 between July 2020 and January 2021. The diagnosis was made by PCR from nasopharyngeal/oral swabs or bronchoalveolar lavage. Outcomes were classified as: recovered, persistently positive, died.
Results
We identified 116 patients. Median age was 59 years (range 20-92); 55% were male. 13% had no symptoms; 49% had mild disease with no need for oxygen therapy; 14% with moderately severe disease were treated with low flow oxygen therapy; 25% had severe COVID-19 with respiratory failure and/or septic shock. Except for seven palliative patients, severe cases were treated with noninvasive ventilation (3%), mechanical ventilation (13%) and ECMO (1%). 27% received no treatment for COVID-19; 38% were treated with antibiotics, corticosteroids and/or anticoagulant therapy; 34% received remdesivir, 6% in combination with convalescent plasma; 5% were treated with extracorporeal blood purification. 65 patients recovered (56%), 17 are still positive (15%) and 34 (29%) died.
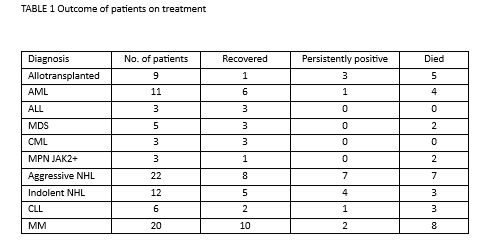
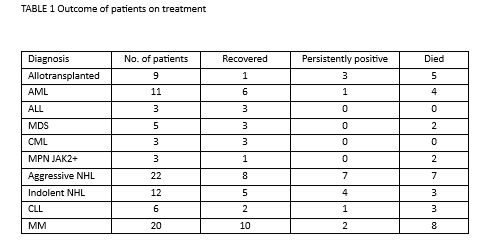
All 4 untreated and 16 patients that were off treatment for more than 3 months recovered. The outcome of those on treatment is presented in Table 1. Allotransplanted patients had the worst outcome, 5 died, 3 are persistently positive and 1 recovered. Untransplanted patients with acute lymphoblastic and chronic myeloid leukemia fared best, 3 out of 3 in each group recovered. Treatment with anti-CD20 monoclonal antibodies (MoAbs) resulted in an increase in persistent positivity, frequently longer than 8 weeks. Of the 34 patients, 9 died, 12 have persistent infection and 13 recovered. There was no clear-cut correlation between outcome and other types of treatment within diagnostic groups.
Conclusion
COVID19 in hematologic patients, who are currently on treatment, follows a significantly worse course than in the general population or other cancer types. Allotransplanted patients have the highest mortality, while those treated with anti-CD20 MoAbs frequently have a persistent infection with dubious outcome.
Keyword(s): COVID-19
Abstract: EP826
Type: E-Poster Presentation
Session title: Infections in hematology (incl. supportive care/therapy)
Background
Reports on outcomes of COVID-19 in hematologic patients vary.
Aims
To describe outcomes and risk factors of SARS-CoV2 infection in patients treated in a large university medical center.
Methods
We analyzed the outcomes of our patients diagnosed with COVID-19 between July 2020 and January 2021. The diagnosis was made by PCR from nasopharyngeal/oral swabs or bronchoalveolar lavage. Outcomes were classified as: recovered, persistently positive, died.
Results
We identified 116 patients. Median age was 59 years (range 20-92); 55% were male. 13% had no symptoms; 49% had mild disease with no need for oxygen therapy; 14% with moderately severe disease were treated with low flow oxygen therapy; 25% had severe COVID-19 with respiratory failure and/or septic shock. Except for seven palliative patients, severe cases were treated with noninvasive ventilation (3%), mechanical ventilation (13%) and ECMO (1%). 27% received no treatment for COVID-19; 38% were treated with antibiotics, corticosteroids and/or anticoagulant therapy; 34% received remdesivir, 6% in combination with convalescent plasma; 5% were treated with extracorporeal blood purification. 65 patients recovered (56%), 17 are still positive (15%) and 34 (29%) died.
All 4 untreated and 16 patients that were off treatment for more than 3 months recovered. The outcome of those on treatment is presented in Table 1. Allotransplanted patients had the worst outcome, 5 died, 3 are persistently positive and 1 recovered. Untransplanted patients with acute lymphoblastic and chronic myeloid leukemia fared best, 3 out of 3 in each group recovered. Treatment with anti-CD20 monoclonal antibodies (MoAbs) resulted in an increase in persistent positivity, frequently longer than 8 weeks. Of the 34 patients, 9 died, 12 have persistent infection and 13 recovered. There was no clear-cut correlation between outcome and other types of treatment within diagnostic groups.
Conclusion
COVID19 in hematologic patients, who are currently on treatment, follows a significantly worse course than in the general population or other cancer types. Allotransplanted patients have the highest mortality, while those treated with anti-CD20 MoAbs frequently have a persistent infection with dubious outcome.
Keyword(s): COVID-19


