
Contributions
Abstract: EP823
Type: E-Poster Presentation
Session title: Infections in hematology (incl. supportive care/therapy)
Background
Patients undergoing allogeneic hematopoietic stem cell transplantation (allo-HSCT) are exposed to a wide range of severe complications. Bloodstream infection (BSI) is an emergency that occurs frequently and is one of the main causes of morbidity and mortality in these patients. Hence, the importance of knowing the principal microorganisms responsible for this complication and therefore, prescribing the most adequate broad-spectrum empirical antibiotic.
Aims
Our main objective is to describe episodes of BSI between days 0 to 100 in patients undergoing allo-HSCT in our center. Our secondary objectives are to analyze the role of prophylactic antibiotic therapy, the impact of inappropriate empirical antibiotic therapy on patients outcome and overall survival (OS) in patients suffering early BSI.
Methods
A one center retrospective study, with data obtained from the electronic clinical history, of the BSI in allo-HSCT in our center from 2015 to 2020. Statistical analysis has been performed with IBM SPSS.19 using appropriate tests for each case.
Results
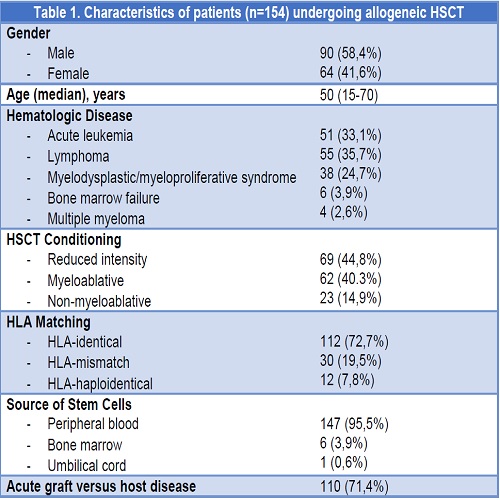
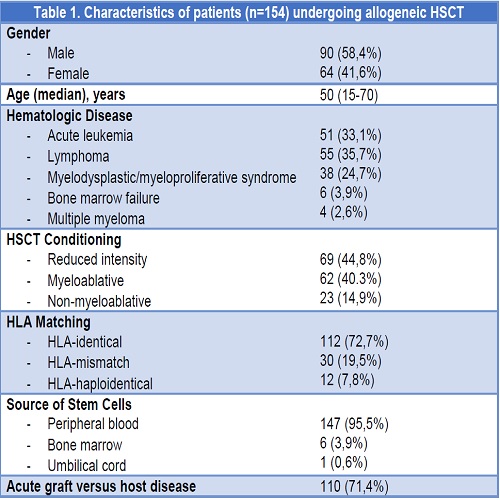
Over the selected period, 154 patients underwent allo-HCST (follow-up median of 329 days), whose main characteristics are summarized on Table 1.
63 episodes of BSI were microbiologically identified in 50 patients (32.5% incidence). 12 patients (7.7%) died as a direct consequence of BSI. Having received allo-HCST, BSI occurred on day 11 (median) and day 51.7 (mean average), range of minimum and maximum values 0-100.
100 patients (64.9%) received prophylactic antibiotics, mostly quinolones (57.1%). 7.8% received early treatment with carbapenems. We were unable to establish a significant relationship between the incidence of BSI in patients who received prophylaxis and those who did not, (chi-square, p=0.7) nor for overall survival rate (logrank, p=0.4).
Gram negative bacilli were the most common group (37 BSI, 58.7%), mainly E. Coli (24 BSI, 38%), with 6 BSI caused by non-fermenting GNB (4 Pseudomonas aer., 6.3%). There were 21 cases of BSI (33%) caused by Gram positives (11 Staphylococcus spp - 7 S. epidermidis and 1 S. aureus -, 7 E. faecium, 1 E. faecalis, and 2 Strept. mitis) and 5 by anaerobic microorganisms.
The majority of BSI (60%) were treated empirically during the first hour with empirical antibiotic monotherapy (carbapenem in 66% of the cases). The empiric antibiotics used for 12 of the episodes of BSI (19%) were inadequate according to the microorganism’s resistance profile, and 5 of them died as a direct consequence of the BSI (overall crude mortality rate due to BSI 7%, mortality rate directly related to inadequate antibiotic 41.6%).
There were statistically significant differences in overall survival (OS) between patients who suffered BSI during the first 100 days post HSCT and those who did not (log-rank-p<0,001).
Conclusion
BSI after HSCT remains a clinical challenge. In our center, one-third of patients develop this complication. Gram negative bacilli are the main germs involved, especially E. coli.
It is absolutely essential to know our environment’s epidemiology and the presence of multi-resistant germs, so as to fit empirical treatment to clinical practice. The use of an inappropriate antibiotic can result in a significant mortality increase.
From our experience, the use of prophylactic antibiotics is not indispensable to decrease the incidence of BSI.
We found significant differences in OS between patients who suffered BSI and those who did not. It is necessary to conduct multivariate studies in order to confirm this hypothesis.
Keyword(s): Allogeneic hematopoietic stem cell transplant, Complications, Infection, Mortality
Abstract: EP823
Type: E-Poster Presentation
Session title: Infections in hematology (incl. supportive care/therapy)
Background
Patients undergoing allogeneic hematopoietic stem cell transplantation (allo-HSCT) are exposed to a wide range of severe complications. Bloodstream infection (BSI) is an emergency that occurs frequently and is one of the main causes of morbidity and mortality in these patients. Hence, the importance of knowing the principal microorganisms responsible for this complication and therefore, prescribing the most adequate broad-spectrum empirical antibiotic.
Aims
Our main objective is to describe episodes of BSI between days 0 to 100 in patients undergoing allo-HSCT in our center. Our secondary objectives are to analyze the role of prophylactic antibiotic therapy, the impact of inappropriate empirical antibiotic therapy on patients outcome and overall survival (OS) in patients suffering early BSI.
Methods
A one center retrospective study, with data obtained from the electronic clinical history, of the BSI in allo-HSCT in our center from 2015 to 2020. Statistical analysis has been performed with IBM SPSS.19 using appropriate tests for each case.
Results
Over the selected period, 154 patients underwent allo-HCST (follow-up median of 329 days), whose main characteristics are summarized on Table 1.
63 episodes of BSI were microbiologically identified in 50 patients (32.5% incidence). 12 patients (7.7%) died as a direct consequence of BSI. Having received allo-HCST, BSI occurred on day 11 (median) and day 51.7 (mean average), range of minimum and maximum values 0-100.
100 patients (64.9%) received prophylactic antibiotics, mostly quinolones (57.1%). 7.8% received early treatment with carbapenems. We were unable to establish a significant relationship between the incidence of BSI in patients who received prophylaxis and those who did not, (chi-square, p=0.7) nor for overall survival rate (logrank, p=0.4).
Gram negative bacilli were the most common group (37 BSI, 58.7%), mainly E. Coli (24 BSI, 38%), with 6 BSI caused by non-fermenting GNB (4 Pseudomonas aer., 6.3%). There were 21 cases of BSI (33%) caused by Gram positives (11 Staphylococcus spp - 7 S. epidermidis and 1 S. aureus -, 7 E. faecium, 1 E. faecalis, and 2 Strept. mitis) and 5 by anaerobic microorganisms.
The majority of BSI (60%) were treated empirically during the first hour with empirical antibiotic monotherapy (carbapenem in 66% of the cases). The empiric antibiotics used for 12 of the episodes of BSI (19%) were inadequate according to the microorganism’s resistance profile, and 5 of them died as a direct consequence of the BSI (overall crude mortality rate due to BSI 7%, mortality rate directly related to inadequate antibiotic 41.6%).
There were statistically significant differences in overall survival (OS) between patients who suffered BSI during the first 100 days post HSCT and those who did not (log-rank-p<0,001).
Conclusion
BSI after HSCT remains a clinical challenge. In our center, one-third of patients develop this complication. Gram negative bacilli are the main germs involved, especially E. coli.
It is absolutely essential to know our environment’s epidemiology and the presence of multi-resistant germs, so as to fit empirical treatment to clinical practice. The use of an inappropriate antibiotic can result in a significant mortality increase.
From our experience, the use of prophylactic antibiotics is not indispensable to decrease the incidence of BSI.
We found significant differences in OS between patients who suffered BSI and those who did not. It is necessary to conduct multivariate studies in order to confirm this hypothesis.
Keyword(s): Allogeneic hematopoietic stem cell transplant, Complications, Infection, Mortality


