
Contributions
Abstract: EP816
Type: E-Poster Presentation
Session title: Infections in hematology (incl. supportive care/therapy)
Background
COVID-19 disease caused by SARS-CoV-2 coronavirus has affected millions of people worldwide. The mortality of this infection varies with age and comorbidities up to more than 10% in very elderly population. The aim of our study was to determine the mortality rate and healthcare utilization among multiple myeloma patients and describe the potential risk factors for death.
Aims
The aim of our study was to determine the mortality rate and healthcare utilization among multiple myeloma patients and describe the potential risk factors for death.
Methods
We retrospectively analyzed entries in the Czech Registry of Monoclonal Gammopathies from patients who were infected with SARS-CoV-2 from March 2020 until January 2021. Demographic data, treatment patterns, comorbidities, symptoms of COVID-19, treatment modalities and healthcare utilization was compared in survivors and non-survivors.
Results
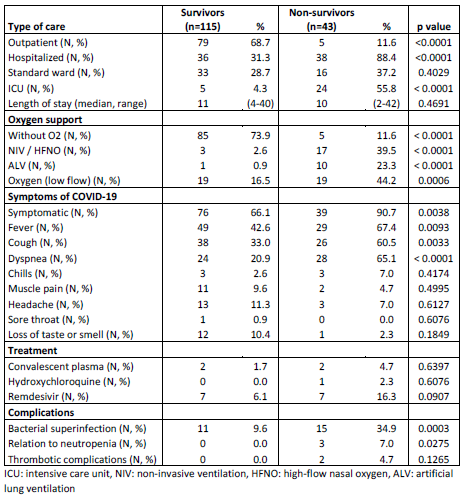
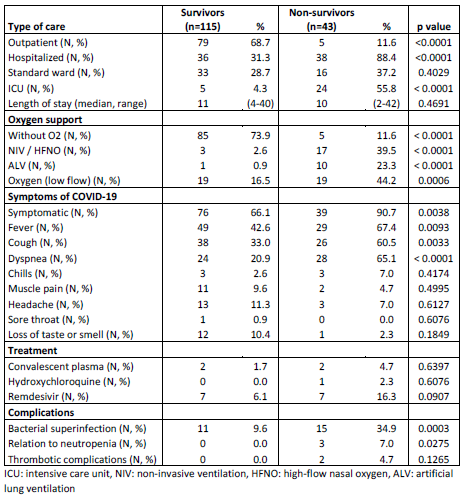
Overall, 158 patients with MM and COVID-19 with known outcome of the infection were identified. There were 72.8% (115/158) survivors and 27.2% (43/158) deceased patients. Both groups were balanced in gender, ECOG, M protein isotype, ISS stage and comorbidities. Non-survivors were significantly older (median 71.5 years vs 67.9 years, p=0.046). There were no differences between previous treatment lines in either group. Patients received median one prior line of therapy (range 0-6, p=0.994). 95% of patients were exposed to IMiDs (150/158), 89.9% to proteasome inhibitors (142/158) and 18.4% (29/158) to anti-CD38 antibody. Autologous stem cell transplantation was used in 36.7% (58/158) of patients. There were no differences in administered treatment in both groups. Inpatient treatment due to COVID-19 was required in 46.8% (74/158) of patients. Survivors hospitalization rate was 31.3% (36/115) and 88.4% (38/43) in non-survivors. In-hospital mortality was 51.4% (38/74). Non-survivors had more intensive care unit stays (4.3% vs 55.8%, p<0.0001) and needed more ventilation support (0.9 % vs 23.3%, p<0.0001). Mortality of patients who needed ICU was 82.8% (24/29 ICU stays) and 32.7% (16/49 ward stays) in patients who needed standard ward inpatient therapy. Mortality of patients needing artificial ventilation was 90.9% (1/11). Mortality of patients needing non-invasive ventilation or high flow nasal oxygen and 85.0% (17/20). Mortality of patients needing low flow nasal oxygen was 50% (19/38). Table 1 shows results in detail.
Conclusion
The mortality of MM patients with COVID-19 was very high especially in patients in need of any type of ventilation support. Healthcare utilization was high with almost half of the infected myeloma patients needing inpatient treatment. No apparent risk factors in terms of disease status or previous treatment were identified.
Supported by MH CZ - DRO (UHHK, 00169906) and by the program PROGRES Q40/8.
Keyword(s): COVID-19, Mortality, Myeloma
Abstract: EP816
Type: E-Poster Presentation
Session title: Infections in hematology (incl. supportive care/therapy)
Background
COVID-19 disease caused by SARS-CoV-2 coronavirus has affected millions of people worldwide. The mortality of this infection varies with age and comorbidities up to more than 10% in very elderly population. The aim of our study was to determine the mortality rate and healthcare utilization among multiple myeloma patients and describe the potential risk factors for death.
Aims
The aim of our study was to determine the mortality rate and healthcare utilization among multiple myeloma patients and describe the potential risk factors for death.
Methods
We retrospectively analyzed entries in the Czech Registry of Monoclonal Gammopathies from patients who were infected with SARS-CoV-2 from March 2020 until January 2021. Demographic data, treatment patterns, comorbidities, symptoms of COVID-19, treatment modalities and healthcare utilization was compared in survivors and non-survivors.
Results
Overall, 158 patients with MM and COVID-19 with known outcome of the infection were identified. There were 72.8% (115/158) survivors and 27.2% (43/158) deceased patients. Both groups were balanced in gender, ECOG, M protein isotype, ISS stage and comorbidities. Non-survivors were significantly older (median 71.5 years vs 67.9 years, p=0.046). There were no differences between previous treatment lines in either group. Patients received median one prior line of therapy (range 0-6, p=0.994). 95% of patients were exposed to IMiDs (150/158), 89.9% to proteasome inhibitors (142/158) and 18.4% (29/158) to anti-CD38 antibody. Autologous stem cell transplantation was used in 36.7% (58/158) of patients. There were no differences in administered treatment in both groups. Inpatient treatment due to COVID-19 was required in 46.8% (74/158) of patients. Survivors hospitalization rate was 31.3% (36/115) and 88.4% (38/43) in non-survivors. In-hospital mortality was 51.4% (38/74). Non-survivors had more intensive care unit stays (4.3% vs 55.8%, p<0.0001) and needed more ventilation support (0.9 % vs 23.3%, p<0.0001). Mortality of patients who needed ICU was 82.8% (24/29 ICU stays) and 32.7% (16/49 ward stays) in patients who needed standard ward inpatient therapy. Mortality of patients needing artificial ventilation was 90.9% (1/11). Mortality of patients needing non-invasive ventilation or high flow nasal oxygen and 85.0% (17/20). Mortality of patients needing low flow nasal oxygen was 50% (19/38). Table 1 shows results in detail.
Conclusion
The mortality of MM patients with COVID-19 was very high especially in patients in need of any type of ventilation support. Healthcare utilization was high with almost half of the infected myeloma patients needing inpatient treatment. No apparent risk factors in terms of disease status or previous treatment were identified.
Supported by MH CZ - DRO (UHHK, 00169906) and by the program PROGRES Q40/8.
Keyword(s): COVID-19, Mortality, Myeloma


