
Contributions
Abstract: EP812
Type: E-Poster Presentation
Session title: Infections in hematology (incl. supportive care/therapy)
Background
The coronavirus disease 2019 (COVID-19), caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) usually resolves with no further complications. However, in some patients, an unbalanced immune response and the occurrence of thrombotic events lead to severe clinical manifestations; with age, gender and comorbidities (namely, arterial hypertension [AHT] or diabetes) as acknowledged risk factors. The clinical management of these hospitalized patients is still a matter of debate, and the effectiveness of certain treatments (angiotensin-converting enzyme 2 inhibitors [ACE2-Is], angiotensin receptor blockers [ARBs], non-steroid anti-inflammatory drugs [NSAIDs], corticosteroids, and low molecular weight heparin [LMWH]) to handle said manifestations and comorbidities has been questioned.
Aims
In this study, we aim to assess the impact of the clinical management of arterial hypertension, inflammation and thrombosis on the survival of COVID-19 patients.
Methods
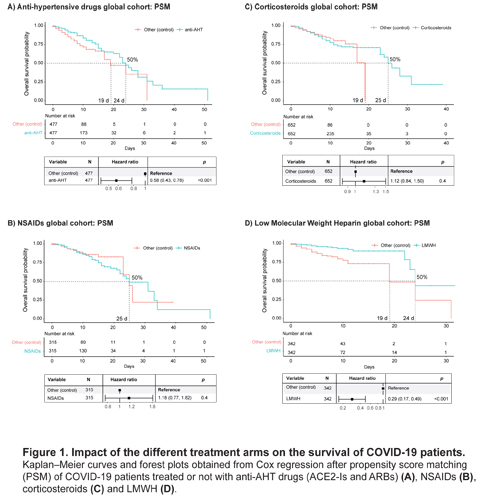
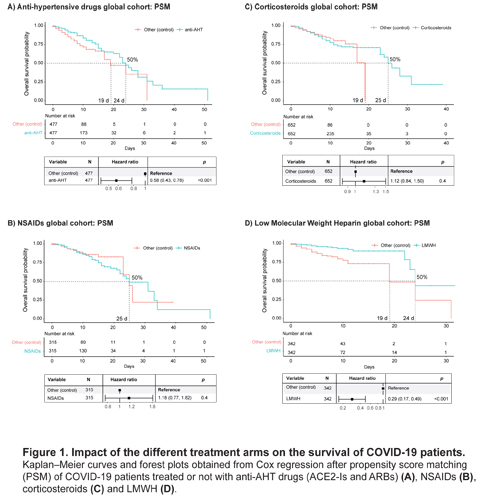
This observational retrospective study is composed of two Spanish cohorts, one from HM Hospitales and another from Hospital Universitario Central de Asturias, with 2035 and 72 laboratory-confirmed COVID-19 adult patients, respectively. The global analysis was performed in the HM cohort after stratification to study the impact of the different treatment arms, having as control group on each arm the respective untreated patients. The HUCA cohort was used as validation of the implementation of thromboprophylaxis in hospitalised patients. The primary end point was the time from hospital admission to discharge or death. Cox proportional-hazards regression, Kaplan-Meier survival curves and propensity score matching were employed, to further control for potential bias and the non-randomized treatment administration. Demographic variables (sex and age), comorbidities (diabetes and AHT), and treatment arms (when opportune) were included as co-variates. All analyses and figures were generated using R software (version 3.6.1).
Results
Cox regression identified age (older), sex (males) and AHT (but not diabetes) as risk variables in the HM cohort. Among the treatment arms of study, all treatment regimens, including LMWH alone or in combination with corticosteroids and anti-AHT drugs, conferred a significant advantage, as opposed to corticosteroids alone or in combination. Furthermore, the management of AHT with ACE2-Is or ARBs is not detrimental, as initially reported, and neither was the use of NSAIDs. On the contrary, our analysis shows that the use of corticosteroids, including dexamethasone, is not beneficial. Importantly, the therapeutic or prophylactic management of thrombosis in COVID-19 patients with LMWH, significantly improves the survival of hospitalized patients.
Conclusion
These results suggest cautiousness when administering corticosteroids for immunosuppression, and whether to limit said administration to the situations that require it (i.e., to facilitate pulmonary capacity as part of the general guidelines in patients with respiratory distress), but not as a protocolized guideline to treat hospitalized COVID-19 patients in general. In particular, dexamethasone may potentially be detrimental to patients in general wards (not critically ill and without respiratory distress). Additionally, they support the effectiveness of thrombosis prophylaxis with LMWH on COVID-19 patients as a first-line treatment, without the need to compromise the treatment of comorbidities.
Keyword(s): Comorbidities, Corticosteroids, COVID-19, Thrombosis
Abstract: EP812
Type: E-Poster Presentation
Session title: Infections in hematology (incl. supportive care/therapy)
Background
The coronavirus disease 2019 (COVID-19), caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) usually resolves with no further complications. However, in some patients, an unbalanced immune response and the occurrence of thrombotic events lead to severe clinical manifestations; with age, gender and comorbidities (namely, arterial hypertension [AHT] or diabetes) as acknowledged risk factors. The clinical management of these hospitalized patients is still a matter of debate, and the effectiveness of certain treatments (angiotensin-converting enzyme 2 inhibitors [ACE2-Is], angiotensin receptor blockers [ARBs], non-steroid anti-inflammatory drugs [NSAIDs], corticosteroids, and low molecular weight heparin [LMWH]) to handle said manifestations and comorbidities has been questioned.
Aims
In this study, we aim to assess the impact of the clinical management of arterial hypertension, inflammation and thrombosis on the survival of COVID-19 patients.
Methods
This observational retrospective study is composed of two Spanish cohorts, one from HM Hospitales and another from Hospital Universitario Central de Asturias, with 2035 and 72 laboratory-confirmed COVID-19 adult patients, respectively. The global analysis was performed in the HM cohort after stratification to study the impact of the different treatment arms, having as control group on each arm the respective untreated patients. The HUCA cohort was used as validation of the implementation of thromboprophylaxis in hospitalised patients. The primary end point was the time from hospital admission to discharge or death. Cox proportional-hazards regression, Kaplan-Meier survival curves and propensity score matching were employed, to further control for potential bias and the non-randomized treatment administration. Demographic variables (sex and age), comorbidities (diabetes and AHT), and treatment arms (when opportune) were included as co-variates. All analyses and figures were generated using R software (version 3.6.1).
Results
Cox regression identified age (older), sex (males) and AHT (but not diabetes) as risk variables in the HM cohort. Among the treatment arms of study, all treatment regimens, including LMWH alone or in combination with corticosteroids and anti-AHT drugs, conferred a significant advantage, as opposed to corticosteroids alone or in combination. Furthermore, the management of AHT with ACE2-Is or ARBs is not detrimental, as initially reported, and neither was the use of NSAIDs. On the contrary, our analysis shows that the use of corticosteroids, including dexamethasone, is not beneficial. Importantly, the therapeutic or prophylactic management of thrombosis in COVID-19 patients with LMWH, significantly improves the survival of hospitalized patients.
Conclusion
These results suggest cautiousness when administering corticosteroids for immunosuppression, and whether to limit said administration to the situations that require it (i.e., to facilitate pulmonary capacity as part of the general guidelines in patients with respiratory distress), but not as a protocolized guideline to treat hospitalized COVID-19 patients in general. In particular, dexamethasone may potentially be detrimental to patients in general wards (not critically ill and without respiratory distress). Additionally, they support the effectiveness of thrombosis prophylaxis with LMWH on COVID-19 patients as a first-line treatment, without the need to compromise the treatment of comorbidities.
Keyword(s): Comorbidities, Corticosteroids, COVID-19, Thrombosis


