
Contributions
Abstract: EP811
Type: E-Poster Presentation
Session title: Infections in hematology (incl. supportive care/therapy)
Background
Infections in patients suffering from myelodysplastic syndromes (MDS) have a negative impact on quality of life, health care costs and are associated with mortality. Little is known about the burden of infections in MDS patients. Current estimates of infection rates are based on results from clinical trials or retrospective analyses that only reviewed hospital records. There are no population-based real-world studies that investigate the burden of infections by the use of anti-infective agents in MDS patients in first and second line care.
Aims
The primary objective of this study was to analyse the increase in susceptibility for infections in patients diagnosed with MDS. Therefore, the prescriptions of anti-infective agents in Dutch MDS patients, both before and after diagnosis of MDS, were collected. Dutch policies on prescribing anti-infective agents are strict and therefore are an accurate reflection of infection rates.
Methods
We performed an observational, population-based study using the HemoBase population registry, including all MDS patients diagnosed between 2005 and 2017 in Friesland, a Dutch province with circa 650.000 inhabitants (Rozema et al. (2021), accepted, Blood Advances). Informed consent was obtained. Community pharmacies provided information about the use of anti-infective agents from 10 years before MDS diagnosis to end of follow-up (Dec. 2020). These data were combined with HemoBase registry data. Results were presented as prescriptions/year, treatment days/year or defined daily dose per 1000 patient days (DID). Descriptive analyses and Wilcoxon Signed Rank tests were performed using IBM SPSS version 24.
Results
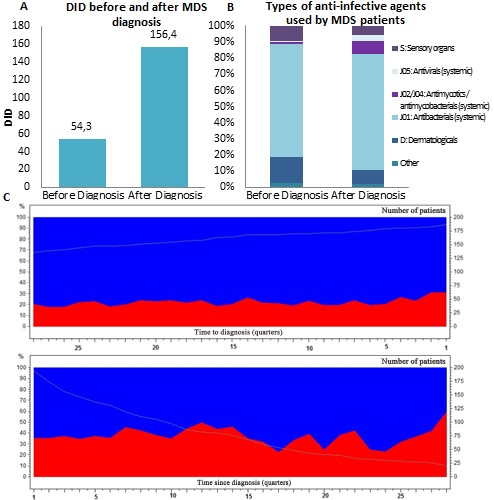
A total of 292 MDS patients were identified, of whom in 201 patients (70%) information on prescribed anti-infective agents was obtained. The response rate was 91.4% for pharmacists and 56.5% for dispensing general practitioners. Patients received significantly more prescriptions/year after diagnosis (median 2.5; 95% CI: 2.1-3.0) than before diagnosis (median 0.8; 95% CI: 0.7-1.0; p<0.01). Likewise, the number of treatment days/year significantly increased (p<0.01) from a median of 7.7 (95% CI: 5.4-10.2) treatment days/year before diagnosis to 23.7 (95% CI: 16.8-31.0) after diagnosis. This corresponds to 54.3 DID (95% CI: 53.7-55.0) before diagnosis and 156.4 DID (95% CI: 154.6-158.2) after diagnosis (rate ratio: 2.9 (95% CI: 2.8-2.9); p<0.01, Fig. 1A). As shown in figure 1C, the prescriptions gradually increased over time. Patients with high-risk MDS did not seem to use more anti-infective agents than low-risk MDS patients (p=0.27). Before diagnosis, 26 patients (12.9%) were admitted to hospital due to an infection, compared to 78 patients (38.8%) after diagnosis; the rate ratio for an infection-related hospital admission was 3.0 (95% CI: 1.9-4.7). Patients mostly received antibacterial agents for systemic use (ATC group J01): 69.6% before diagnosis and 71.3% after diagnosis (Fig. 1B).
Conclusion
This study showed a significantly increased use of anti-infective agents in patients after diagnosis of MDS in both low-risk and high-risk MDS patients. After the diagnosis MDS, patients had a 3-fold higher risk for infections in an outpatient setting and a 3-fold higher chance for an infection-related hospital admission compared to before MDS diagnosis. To our knowledge, this is the first descriptive population-based study that provides an overall insight in prescribed anti-infective agents both in- and outside the clinical setting in a well-defined representative MDS patient cohort.
Keyword(s): Infection, Myelodysplasia, Population
Abstract: EP811
Type: E-Poster Presentation
Session title: Infections in hematology (incl. supportive care/therapy)
Background
Infections in patients suffering from myelodysplastic syndromes (MDS) have a negative impact on quality of life, health care costs and are associated with mortality. Little is known about the burden of infections in MDS patients. Current estimates of infection rates are based on results from clinical trials or retrospective analyses that only reviewed hospital records. There are no population-based real-world studies that investigate the burden of infections by the use of anti-infective agents in MDS patients in first and second line care.
Aims
The primary objective of this study was to analyse the increase in susceptibility for infections in patients diagnosed with MDS. Therefore, the prescriptions of anti-infective agents in Dutch MDS patients, both before and after diagnosis of MDS, were collected. Dutch policies on prescribing anti-infective agents are strict and therefore are an accurate reflection of infection rates.
Methods
We performed an observational, population-based study using the HemoBase population registry, including all MDS patients diagnosed between 2005 and 2017 in Friesland, a Dutch province with circa 650.000 inhabitants (Rozema et al. (2021), accepted, Blood Advances). Informed consent was obtained. Community pharmacies provided information about the use of anti-infective agents from 10 years before MDS diagnosis to end of follow-up (Dec. 2020). These data were combined with HemoBase registry data. Results were presented as prescriptions/year, treatment days/year or defined daily dose per 1000 patient days (DID). Descriptive analyses and Wilcoxon Signed Rank tests were performed using IBM SPSS version 24.
Results
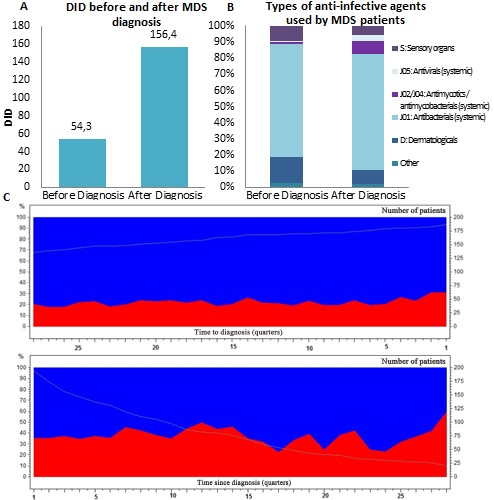
A total of 292 MDS patients were identified, of whom in 201 patients (70%) information on prescribed anti-infective agents was obtained. The response rate was 91.4% for pharmacists and 56.5% for dispensing general practitioners. Patients received significantly more prescriptions/year after diagnosis (median 2.5; 95% CI: 2.1-3.0) than before diagnosis (median 0.8; 95% CI: 0.7-1.0; p<0.01). Likewise, the number of treatment days/year significantly increased (p<0.01) from a median of 7.7 (95% CI: 5.4-10.2) treatment days/year before diagnosis to 23.7 (95% CI: 16.8-31.0) after diagnosis. This corresponds to 54.3 DID (95% CI: 53.7-55.0) before diagnosis and 156.4 DID (95% CI: 154.6-158.2) after diagnosis (rate ratio: 2.9 (95% CI: 2.8-2.9); p<0.01, Fig. 1A). As shown in figure 1C, the prescriptions gradually increased over time. Patients with high-risk MDS did not seem to use more anti-infective agents than low-risk MDS patients (p=0.27). Before diagnosis, 26 patients (12.9%) were admitted to hospital due to an infection, compared to 78 patients (38.8%) after diagnosis; the rate ratio for an infection-related hospital admission was 3.0 (95% CI: 1.9-4.7). Patients mostly received antibacterial agents for systemic use (ATC group J01): 69.6% before diagnosis and 71.3% after diagnosis (Fig. 1B).
Conclusion
This study showed a significantly increased use of anti-infective agents in patients after diagnosis of MDS in both low-risk and high-risk MDS patients. After the diagnosis MDS, patients had a 3-fold higher risk for infections in an outpatient setting and a 3-fold higher chance for an infection-related hospital admission compared to before MDS diagnosis. To our knowledge, this is the first descriptive population-based study that provides an overall insight in prescribed anti-infective agents both in- and outside the clinical setting in a well-defined representative MDS patient cohort.
Keyword(s): Infection, Myelodysplasia, Population


