
Contributions
Abstract: EP808
Type: E-Poster Presentation
Session title: Indolent and mantle-cell non-Hodgkin lymphoma - Clinical
Background
FLIPI is the most frequently used prognostic tool even nowadays, although it was developed in the pre-Rituximab (R) era with overall survival (OS) as the endpoint. It has not been extensively studied, whether it can predict progression free survival (PFS) and if it still has a strong prognostic value for OS in R-treated patients, especially outside clinical trials.
Aims
To identify prognostic factors and examine the prognostic significance of FLIPI in a series of FL patients, treated in the R era outside clinical trials
Methods
282 consecutive patients with FL diagnosed and treated between 2000 and 2020 from a single Unit were retrospectively studied. Several prognostic parameters were analyzed for OS, PFS and disease-specific survival (DSS).
Results
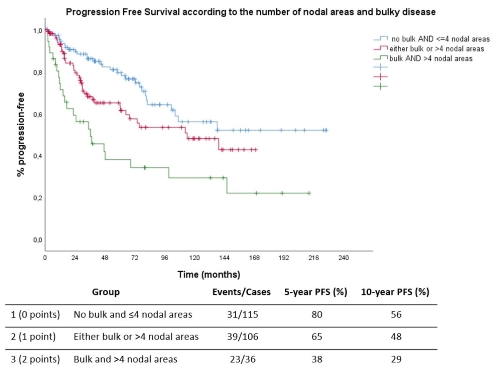
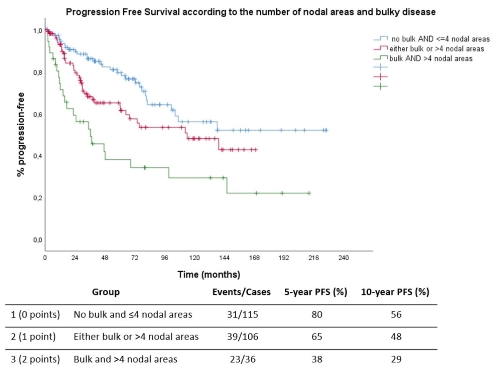
112 patients (40%) were males with a median age of 56.7 years. 206 cases had histologic grade 1/2 (73%) and the remaining 76 (27%) grade 3A. The distribution of clinical stages was as follows: 71 (25%) stage 1, 35 (13%) stage 2, 42 (15%) stage 3, 132 (47%) stage 4; 12% had B symptoms, 21% elevated LDH, 25% bulky disease (>7 cm), 7% had peripheral blood involvement and 41% had bone marrow involvement. 43% had >4 involved nodal areas. The most frequent treatment was R non-anthracycline chemotherapy, followed by RCHOP; 61% received maintenance after first line treatment. Median PFS was 114 months; 5- and 10-year PFS were 67.5% and 49%, respectively. For PFS, FLIPI score was not significant, whereas, bulky disease (p<0.0001) and number of nodal areas (p=0.018) were the only significant factors by univariate analysis; bulky disease remained significant by multivariate analysis (p<0.0001). A simple score based on nodal areas (0 points for ≤4 vs 1 point for >4) and bulky disease (0 points for no bulk vs 1 point for bulk) could stratify patients into three groups with a significantly different PFS (p<0.0001, figure). FLIPI score was prognostic for OS (p<0.0001) and DSS (P=0.004), but low- and intermediate risk groups had similar outcomes, especially for DSS. When low-and intermediate risk groups were grouped together (FLIPI 0-2) against high-risk (FLIPI 3-5), 5- and 10- year OS was 95% and 90.4% for FLIPI 0-2 vs 76% and 59% for FLIPI 3-5. 5- and 10- year DSS were both 96% for FLIPI 0-2 vs 90% and 76% for FLIPI 3-5. Considering the 5 parameters of FLIPI and bulky disease, by multivariate analysis, hemoglobin, age and bulky disease were the ones that were significant for OS, whereas, only bulky disease was significant for DSS.
Conclusion
In real world, outside clinical trials, with the observed improvement of survival of patients with FL in the R-era, FLIPI is still prognostic for OS, but may have limited predictive capacity for PFS. Bulky disease seems to be a potent marker for PFS, OS and DSS and should be further integrated and validated in easily applicable prognostic scores.
Keyword(s): Follicular lymphoma, Prognostic factor
Abstract: EP808
Type: E-Poster Presentation
Session title: Indolent and mantle-cell non-Hodgkin lymphoma - Clinical
Background
FLIPI is the most frequently used prognostic tool even nowadays, although it was developed in the pre-Rituximab (R) era with overall survival (OS) as the endpoint. It has not been extensively studied, whether it can predict progression free survival (PFS) and if it still has a strong prognostic value for OS in R-treated patients, especially outside clinical trials.
Aims
To identify prognostic factors and examine the prognostic significance of FLIPI in a series of FL patients, treated in the R era outside clinical trials
Methods
282 consecutive patients with FL diagnosed and treated between 2000 and 2020 from a single Unit were retrospectively studied. Several prognostic parameters were analyzed for OS, PFS and disease-specific survival (DSS).
Results
112 patients (40%) were males with a median age of 56.7 years. 206 cases had histologic grade 1/2 (73%) and the remaining 76 (27%) grade 3A. The distribution of clinical stages was as follows: 71 (25%) stage 1, 35 (13%) stage 2, 42 (15%) stage 3, 132 (47%) stage 4; 12% had B symptoms, 21% elevated LDH, 25% bulky disease (>7 cm), 7% had peripheral blood involvement and 41% had bone marrow involvement. 43% had >4 involved nodal areas. The most frequent treatment was R non-anthracycline chemotherapy, followed by RCHOP; 61% received maintenance after first line treatment. Median PFS was 114 months; 5- and 10-year PFS were 67.5% and 49%, respectively. For PFS, FLIPI score was not significant, whereas, bulky disease (p<0.0001) and number of nodal areas (p=0.018) were the only significant factors by univariate analysis; bulky disease remained significant by multivariate analysis (p<0.0001). A simple score based on nodal areas (0 points for ≤4 vs 1 point for >4) and bulky disease (0 points for no bulk vs 1 point for bulk) could stratify patients into three groups with a significantly different PFS (p<0.0001, figure). FLIPI score was prognostic for OS (p<0.0001) and DSS (P=0.004), but low- and intermediate risk groups had similar outcomes, especially for DSS. When low-and intermediate risk groups were grouped together (FLIPI 0-2) against high-risk (FLIPI 3-5), 5- and 10- year OS was 95% and 90.4% for FLIPI 0-2 vs 76% and 59% for FLIPI 3-5. 5- and 10- year DSS were both 96% for FLIPI 0-2 vs 90% and 76% for FLIPI 3-5. Considering the 5 parameters of FLIPI and bulky disease, by multivariate analysis, hemoglobin, age and bulky disease were the ones that were significant for OS, whereas, only bulky disease was significant for DSS.
Conclusion
In real world, outside clinical trials, with the observed improvement of survival of patients with FL in the R-era, FLIPI is still prognostic for OS, but may have limited predictive capacity for PFS. Bulky disease seems to be a potent marker for PFS, OS and DSS and should be further integrated and validated in easily applicable prognostic scores.
Keyword(s): Follicular lymphoma, Prognostic factor


