
Contributions
Abstract: EP803
Type: E-Poster Presentation
Session title: Indolent and mantle-cell non-Hodgkin lymphoma - Clinical
Background
Some population-based studies demonstrate that the improved longevity of patients with follicular lymphoma (FL) is offset by an increased risk of a variety of second primary malignancies (SPMs) compared to the general population. Awareness about the incidence of SPMs in patients with FL is important to mitigate potential sequelae of SPMs.
Aims
To complement and extend on the sparse literature on SPM development in FL, this nationwide population-based study aimed to assess the risk to develop SPMs in patients with FL in the Netherlands diagnosed during a 30-year period.
Methods
We selected all patients diagnosed with FL grades 1-3B between 1989-2018 from the Netherlands Cancer Registry (NCR) and followed these patients until SPM development, death, or end of follow-up (December 31, 2018), whichever occurred first. Standardized incidence ratios (SIRs) for all SPMs combined—except for basal and squamous cell carcinomas—and specific subtypes of SPMs were calculated by dividing the number of observed malignancies by the expected number of malignancies in an age, sex, and period matched population from the NCR. Synchronous malignancies diagnosed within six months from FL diagnosis (n=248; 1.8% of the total FL population) were excluded to minimize detection bias. We assigned 95% confidence intervals (CIs) for the SIRs by assuming a Poisson distribution for the number of observed SPMs.
Results
We included 13,656 FL patients (median age, 62 years, 49% females) in this study, of whom 1,415 patients (10%) developed at least one SPM after a median follow-up of 5.2 years from diagnosis (interquartile range (IQR), 2.0-10.2 years) at a median age of 69 years (IQR, 62-75 years). Of the 1,415 patients, 550 patients (38%), 432 patients (31%), and 432 patients (31%) were diagnosed with an SPM at 0.5-5, 5-10, and 10-30 years from diagnosis. The cumulative incidence of SPMs was 7.3% (95% CI, 6.8-7.8%) and 14.9% (95% CI, 14.1-15.8%) at 5 and 10 years, respectively.
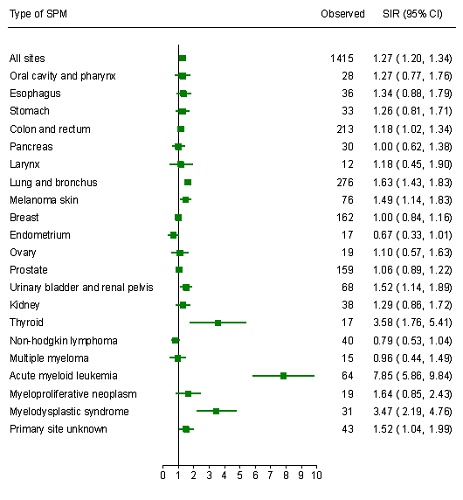
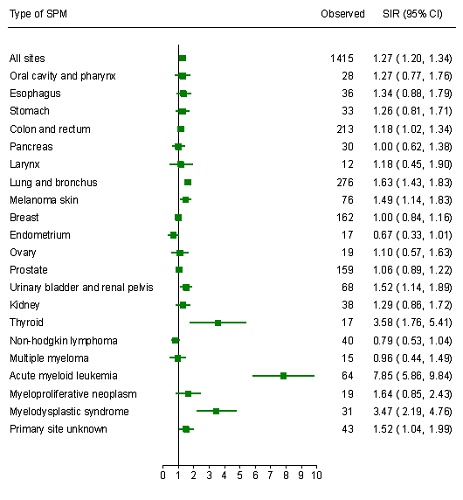
The risk of developing an SPM for patients with FL was statistically significantly elevated compared to the general population with a SIR of 1.27 (95% CI, 1.20-1.34; Figure 1), irrespective of sex. The increased risk was more pronounced among patients 18-60 years at diagnosis (SIR, 1.52; 95% CI, 1.40-1.64) compared to patients >60 years at diagnosis (SIR, 1.10; 95% CI, 1.02-1.18), possibly due to a higher baseline risk among patients 18-60 years. The excess risk of SPMs diminished, albeit it did not disappear, among patients diagnosed in the post-rituximab era (>2002) compared to patients diagnosed in the pre-rituximab era (SIR, 1.15; 95% CI, 1.07-1.24 and SIR, 1.38; 95% CI, 1.28-1.49, respectively). A significantly greater risk was observed for acute myeloid leukemia (7.85), and myelodysplastic syndrome (3.47), and solid tumors of the following sites: thyroid (3.58), lung and bronchus (1.63), primary site unknown (1.52), urinary bladder and renal pelvis (1.52), melanoma of the skin (1.49), and colon and rectum (1.18; Figure 1).
Conclusion
This nationwide, population-based study demonstrates that FL patients have a 1.27 times greater risk of SPMs than the general population that persists for patients diagnosed in the rituximab era. SPMs could reflect late sequelae of treatment or the effect of shared etiologic factors, environmental exposures, and host characteristics. Surveillance of SPMs among FL survivors can be considered in the survivorship care of these patients—particularly among patients aged 18-60 years at diagnosis—to prevent SPMs or reduce the impact of SPMs.
Keyword(s):
Abstract: EP803
Type: E-Poster Presentation
Session title: Indolent and mantle-cell non-Hodgkin lymphoma - Clinical
Background
Some population-based studies demonstrate that the improved longevity of patients with follicular lymphoma (FL) is offset by an increased risk of a variety of second primary malignancies (SPMs) compared to the general population. Awareness about the incidence of SPMs in patients with FL is important to mitigate potential sequelae of SPMs.
Aims
To complement and extend on the sparse literature on SPM development in FL, this nationwide population-based study aimed to assess the risk to develop SPMs in patients with FL in the Netherlands diagnosed during a 30-year period.
Methods
We selected all patients diagnosed with FL grades 1-3B between 1989-2018 from the Netherlands Cancer Registry (NCR) and followed these patients until SPM development, death, or end of follow-up (December 31, 2018), whichever occurred first. Standardized incidence ratios (SIRs) for all SPMs combined—except for basal and squamous cell carcinomas—and specific subtypes of SPMs were calculated by dividing the number of observed malignancies by the expected number of malignancies in an age, sex, and period matched population from the NCR. Synchronous malignancies diagnosed within six months from FL diagnosis (n=248; 1.8% of the total FL population) were excluded to minimize detection bias. We assigned 95% confidence intervals (CIs) for the SIRs by assuming a Poisson distribution for the number of observed SPMs.
Results
We included 13,656 FL patients (median age, 62 years, 49% females) in this study, of whom 1,415 patients (10%) developed at least one SPM after a median follow-up of 5.2 years from diagnosis (interquartile range (IQR), 2.0-10.2 years) at a median age of 69 years (IQR, 62-75 years). Of the 1,415 patients, 550 patients (38%), 432 patients (31%), and 432 patients (31%) were diagnosed with an SPM at 0.5-5, 5-10, and 10-30 years from diagnosis. The cumulative incidence of SPMs was 7.3% (95% CI, 6.8-7.8%) and 14.9% (95% CI, 14.1-15.8%) at 5 and 10 years, respectively.
The risk of developing an SPM for patients with FL was statistically significantly elevated compared to the general population with a SIR of 1.27 (95% CI, 1.20-1.34; Figure 1), irrespective of sex. The increased risk was more pronounced among patients 18-60 years at diagnosis (SIR, 1.52; 95% CI, 1.40-1.64) compared to patients >60 years at diagnosis (SIR, 1.10; 95% CI, 1.02-1.18), possibly due to a higher baseline risk among patients 18-60 years. The excess risk of SPMs diminished, albeit it did not disappear, among patients diagnosed in the post-rituximab era (>2002) compared to patients diagnosed in the pre-rituximab era (SIR, 1.15; 95% CI, 1.07-1.24 and SIR, 1.38; 95% CI, 1.28-1.49, respectively). A significantly greater risk was observed for acute myeloid leukemia (7.85), and myelodysplastic syndrome (3.47), and solid tumors of the following sites: thyroid (3.58), lung and bronchus (1.63), primary site unknown (1.52), urinary bladder and renal pelvis (1.52), melanoma of the skin (1.49), and colon and rectum (1.18; Figure 1).
Conclusion
This nationwide, population-based study demonstrates that FL patients have a 1.27 times greater risk of SPMs than the general population that persists for patients diagnosed in the rituximab era. SPMs could reflect late sequelae of treatment or the effect of shared etiologic factors, environmental exposures, and host characteristics. Surveillance of SPMs among FL survivors can be considered in the survivorship care of these patients—particularly among patients aged 18-60 years at diagnosis—to prevent SPMs or reduce the impact of SPMs.
Keyword(s):


