
Contributions
Abstract: EP704
Type: E-Poster Presentation
Session title: Enzymopathies, membranopathies and other anemias
Background
Autoimmun hemolytic anemia (AIHA) is characterized with autoantibodies that target normal red blood cell membrane antigens and induce cell lysis. Although there have been both pediatric and adult patients with AIHA, its presentation in childhood is relatively rare. Based on this, treatment responses and clinical findings of children with AIHA are very important.
Aims
In this study, we aimed to evaluate the treatment responses and clinical features of pediatric patients with AIHA who were followed up in our center.
Methods
This is a 12 years retrospective cohort study of warm AIHA case collected at Hematology and Oncology Clinic of Dr. Behcet Uz Children’s Hospital. We included 39 patients aged between 1 month and 18 years. These patients’ demographic characteristics, laboratory findings at diagnosis and treatment responses were recorded. Patients with underlying immunodeficiency or autoimmune disease were classified as secondary AIHA, and the other patients as idiopathic AIHA. Idiopathic and secondary autoimmune hemolytic anemia groups were compared in terms of recurrence. The patients groups according to first-line treatment selection were also compared in respect of recurrence.
Results
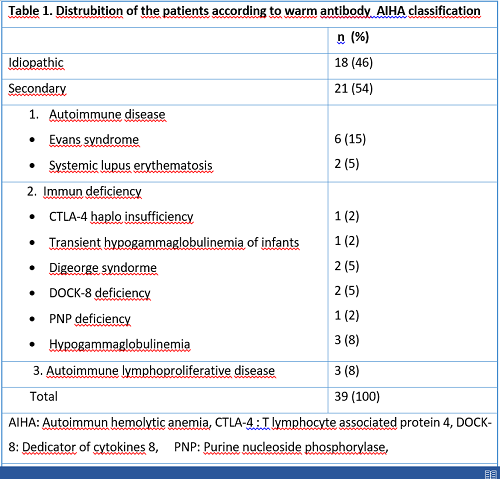
Thirty-nine patients with warm AIHA were collected 16 (41%) girls and 23 (59%) boys. The mean age at diagnosis was 5.1 ± 4.5 years and the mean follow-up period from diagnosis was 7.2 ± 5.9 years. Distrubition of the patients according to classification is seen table 1. Twelve (30.7%) patients reported consanguinity and viral etiology was detected in four (10.2%) patients. At the time of diagnosis, 6 patients received IVIG, 17 patients received steroid, 15 patients received IVIG + steroid combined therapy and only one patient didn’t need treatment. Twenty-three (59%) of them required blood transfusions with a mean hemoglobin level of 5,40 ± 1,83 g/dl. The mean hemoglobin level of 16 (41%) patients who were not transfused at diagnosis was 7,67 ± 1,92 g/dl. According to response criteria 19 (48.7%) of the patients had complete response, 19 (48.7%) had partial response, and one patient (2.6%) was unresponsive. There weren’t difference among the 3 groups of patients who were received IVIG, steroid or IVIG + steroid combined therapy in terms of recurrence during diagnosis (p = 0.128). There were 18 (46.2%) and 2 (5.1%) patients in the secondary and idiopathic AIHA groups who relapsed after treatment response at the time of diagnosis, respectively (p <0.001). During follow up additional therapies which include cyclosporine (n=7), mycophenolate mofetil (n=7), rituximab (n=3) sirolimus (n=2) and danazol (n=1) were applied. Four (10.2%) patients were splenectomised. Two patients ( DOCK 8 deficiency and Digeorge syndrome) died.
Conclusion
This study highlights heterogenity, severity and response rate of first line therapy in pediatric patients with warm AIHA. First line therapy with steroids is effective. However challenges in management of reccurent case remain unresolved. Thus the findings in this study may contributed to clinical features of recurrence in pediatric patients with warm reactive AIHA.
Keyword(s): Anemia, Antibody, Autoimmune hemolytic anemia (AIHA), Recurrence
Abstract: EP704
Type: E-Poster Presentation
Session title: Enzymopathies, membranopathies and other anemias
Background
Autoimmun hemolytic anemia (AIHA) is characterized with autoantibodies that target normal red blood cell membrane antigens and induce cell lysis. Although there have been both pediatric and adult patients with AIHA, its presentation in childhood is relatively rare. Based on this, treatment responses and clinical findings of children with AIHA are very important.
Aims
In this study, we aimed to evaluate the treatment responses and clinical features of pediatric patients with AIHA who were followed up in our center.
Methods
This is a 12 years retrospective cohort study of warm AIHA case collected at Hematology and Oncology Clinic of Dr. Behcet Uz Children’s Hospital. We included 39 patients aged between 1 month and 18 years. These patients’ demographic characteristics, laboratory findings at diagnosis and treatment responses were recorded. Patients with underlying immunodeficiency or autoimmune disease were classified as secondary AIHA, and the other patients as idiopathic AIHA. Idiopathic and secondary autoimmune hemolytic anemia groups were compared in terms of recurrence. The patients groups according to first-line treatment selection were also compared in respect of recurrence.
Results
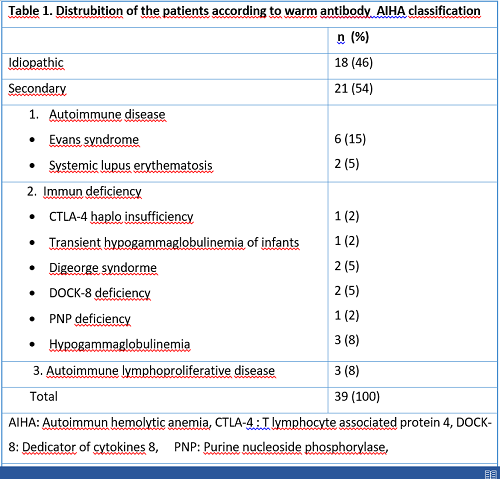
Thirty-nine patients with warm AIHA were collected 16 (41%) girls and 23 (59%) boys. The mean age at diagnosis was 5.1 ± 4.5 years and the mean follow-up period from diagnosis was 7.2 ± 5.9 years. Distrubition of the patients according to classification is seen table 1. Twelve (30.7%) patients reported consanguinity and viral etiology was detected in four (10.2%) patients. At the time of diagnosis, 6 patients received IVIG, 17 patients received steroid, 15 patients received IVIG + steroid combined therapy and only one patient didn’t need treatment. Twenty-three (59%) of them required blood transfusions with a mean hemoglobin level of 5,40 ± 1,83 g/dl. The mean hemoglobin level of 16 (41%) patients who were not transfused at diagnosis was 7,67 ± 1,92 g/dl. According to response criteria 19 (48.7%) of the patients had complete response, 19 (48.7%) had partial response, and one patient (2.6%) was unresponsive. There weren’t difference among the 3 groups of patients who were received IVIG, steroid or IVIG + steroid combined therapy in terms of recurrence during diagnosis (p = 0.128). There were 18 (46.2%) and 2 (5.1%) patients in the secondary and idiopathic AIHA groups who relapsed after treatment response at the time of diagnosis, respectively (p <0.001). During follow up additional therapies which include cyclosporine (n=7), mycophenolate mofetil (n=7), rituximab (n=3) sirolimus (n=2) and danazol (n=1) were applied. Four (10.2%) patients were splenectomised. Two patients ( DOCK 8 deficiency and Digeorge syndrome) died.
Conclusion
This study highlights heterogenity, severity and response rate of first line therapy in pediatric patients with warm AIHA. First line therapy with steroids is effective. However challenges in management of reccurent case remain unresolved. Thus the findings in this study may contributed to clinical features of recurrence in pediatric patients with warm reactive AIHA.
Keyword(s): Anemia, Antibody, Autoimmune hemolytic anemia (AIHA), Recurrence


