
Contributions
Abstract: EP701
Type: E-Poster Presentation
Session title: Enzymopathies, membranopathies and other anemias
Background
Hereditary spherocytosis (HS) is a genetic disorder due to red cell membrane protein abnormalities, characterized by chronic and acute hemolytic anemia of variable degrees of severity. Extramedullary hematopoiesis is a rare complication, which has been reported in several single case reports. It is diagnosed through compressive complications or found incidentally at radiographic controls. Bone marrow reconversion, process in which the yellow marrow is transformed back to red marrow in adults, is observed in various pathological situations such as medullary infiltration by oncological blood diseases (lymphomas, leukemias, myelomas, myelofibrosis), in patients receiving hematopoietic growth factors or in thalassemia and sickle cell anemia. It is not known as a common complication in HS. Here we describe for the first time bone marrow reconversion in two unrelated HS patients complaining with disabling knee pain.
Aims
Study clinical manifestations and genetic characteristics of patients with bone marrow complications in our cohort of HS patients.
Methods
We retrospectively collected clinical and biological data from a total of 137 pediatric or adult HS patients (79 females/58 males; median age at diagnosis 12.4 years, (1day-63 years)) followed in our Center, including genetic analyses of genes implicated in red cell membrane disorders. We focused on bone marrow complications, especially extramedullary hematopoiesis and bone marrow reconversion, based on the available radiological data.
Results
We found no case of extramedullary hematopoiesis in this cohort. By contrast, 2 unrelated patients were diagnosed with bone marrow reconversion at the knees. The first one was a 24-years-old male who complained of knee pain during sports activities. MRI found an iliotibial band syndrome and a knee bone marrow reconversion. This led to the diagnosis of fully compensated hemolysis (Hb 137 g/l, reticulocytes: 381G/L), which was confirmed to be HS in our center, using pink test, EMA test and ektacytometry. NGS analyses showed that the patient bore a known SPTB frameshift mutation SPTB:p.Lys1337Serfs*3.
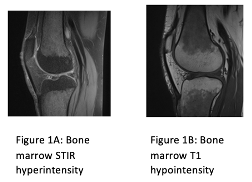
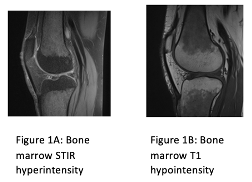
After this unusual presentation, a second patient, a 59-year-old woman diagnosed with HS at the age of 11, following the fortuitous discovery of anemia, consulted in our center for the follow up of her disorder. She also had fully compensated hemolysis (hb 123 g/L, reticulocytes 513 G/l). She was not a heavy smoker. She had been complaining of chronic knee pain for several months. Again, MRI, found a typical bilateral bone marrow reconversion, with decreased T1 signal intensity and STIR hyperintensity in tibial and femoral diaphysis bone marrow, respecting epiphyses (Figure). The patient bore a potentially pathogeneous splice mutation disrupting the splice branch point of intron 38 of the ANK1 gene: ANK1: c.5097-.
Conclusion
Unlike extramedullary hematopoiesis, bone marrow reconversion is an unrecognized bone marrow complication in HS. Extramedullary hematopoiesis is described in HS as mainly mediastinal, paravertebral, renal and splenic masses. Bone marrow reconversion found in 2 patients of this series should be searched more systematically in HS patients. It could be a common and underestimated process leading to chronic and disabling pain in HS patients. Apart from pain medication, the targeted management of this complication requires further investigations in non-anemic patients.
Keyword(s): Bone Marrow, Hereditary spherocytosis, MRI
Abstract: EP701
Type: E-Poster Presentation
Session title: Enzymopathies, membranopathies and other anemias
Background
Hereditary spherocytosis (HS) is a genetic disorder due to red cell membrane protein abnormalities, characterized by chronic and acute hemolytic anemia of variable degrees of severity. Extramedullary hematopoiesis is a rare complication, which has been reported in several single case reports. It is diagnosed through compressive complications or found incidentally at radiographic controls. Bone marrow reconversion, process in which the yellow marrow is transformed back to red marrow in adults, is observed in various pathological situations such as medullary infiltration by oncological blood diseases (lymphomas, leukemias, myelomas, myelofibrosis), in patients receiving hematopoietic growth factors or in thalassemia and sickle cell anemia. It is not known as a common complication in HS. Here we describe for the first time bone marrow reconversion in two unrelated HS patients complaining with disabling knee pain.
Aims
Study clinical manifestations and genetic characteristics of patients with bone marrow complications in our cohort of HS patients.
Methods
We retrospectively collected clinical and biological data from a total of 137 pediatric or adult HS patients (79 females/58 males; median age at diagnosis 12.4 years, (1day-63 years)) followed in our Center, including genetic analyses of genes implicated in red cell membrane disorders. We focused on bone marrow complications, especially extramedullary hematopoiesis and bone marrow reconversion, based on the available radiological data.
Results
We found no case of extramedullary hematopoiesis in this cohort. By contrast, 2 unrelated patients were diagnosed with bone marrow reconversion at the knees. The first one was a 24-years-old male who complained of knee pain during sports activities. MRI found an iliotibial band syndrome and a knee bone marrow reconversion. This led to the diagnosis of fully compensated hemolysis (Hb 137 g/l, reticulocytes: 381G/L), which was confirmed to be HS in our center, using pink test, EMA test and ektacytometry. NGS analyses showed that the patient bore a known SPTB frameshift mutation SPTB:p.Lys1337Serfs*3.
After this unusual presentation, a second patient, a 59-year-old woman diagnosed with HS at the age of 11, following the fortuitous discovery of anemia, consulted in our center for the follow up of her disorder. She also had fully compensated hemolysis (hb 123 g/L, reticulocytes 513 G/l). She was not a heavy smoker. She had been complaining of chronic knee pain for several months. Again, MRI, found a typical bilateral bone marrow reconversion, with decreased T1 signal intensity and STIR hyperintensity in tibial and femoral diaphysis bone marrow, respecting epiphyses (Figure). The patient bore a potentially pathogeneous splice mutation disrupting the splice branch point of intron 38 of the ANK1 gene: ANK1: c.5097-.
Conclusion
Unlike extramedullary hematopoiesis, bone marrow reconversion is an unrecognized bone marrow complication in HS. Extramedullary hematopoiesis is described in HS as mainly mediastinal, paravertebral, renal and splenic masses. Bone marrow reconversion found in 2 patients of this series should be searched more systematically in HS patients. It could be a common and underestimated process leading to chronic and disabling pain in HS patients. Apart from pain medication, the targeted management of this complication requires further investigations in non-anemic patients.
Keyword(s): Bone Marrow, Hereditary spherocytosis, MRI


