Contributions
Abstract: EP692
Type: E-Poster Presentation
Session title: Enzymopathies, membranopathies and other anemias
Background
Hereditary pyruvate kinase (PK) deficiency results in lifelong hemolytic anemia and several significant comorbidities, the epidemiology of which are not well characterized. Among these is reduced bone mineral density (BMD), which can result in premature osteopenia, osteoporosis, and fractures.
Aims
To better characterize the bone density abnormalities in patients (pts) with PK deficiency, this study evaluated pooled pre-treatment baseline data from 3 clinical trials involving pts with PK deficiency investigating mitapivat (AG-348), an allosteric activator of PK: DRIVE-PK (NCT02476916), ACTIVATE (NCT03548220), and ACTIVATE-T (NCT03559699). This is the first large PK deficiency cohort in which dual-energy x-ray absorptiometry (DXA) scores were systematically and consistently assessed.
Methods
DRIVE-PK is a completed phase 2, global, randomized, open-label study. ACTIVATE is an ongoing phase 3, global, randomized, double-blind, placebo-controlled study. ACTIVATE-T is an ongoing phase 3, global, open-label, single-arm study. In all 3 studies, pts ≥18 years (yrs) of age with a confirmed diagnosis of PK deficiency were eligible to participate. Pts were eligible to participate in DRIVE-PK and in ACTIVATE if they were not regularly transfused (DRIVE-PK: ≤3 units of red blood cells in the prior 12 months [mos]; no transfusions in the prior 4 mos; ACTIVATE: ≤4 transfusion episodes in the previous yr; no transfusions in the prior 3 mos) and in ACTIVATE-T if they were regularly transfused (≥6 transfusion episodes in the previous yr). BMD was measured using DXA at baseline; scans were obtained locally for all 3 studies. Scans were interpreted locally for DRIVE-PK and centrally for ACTIVATE and ACTIVATE-T. Osteopenia and osteoporosis were identified on DXA according to standard definitions, and prevalence of each was compared to prevalence ascertained via medical history.
Results
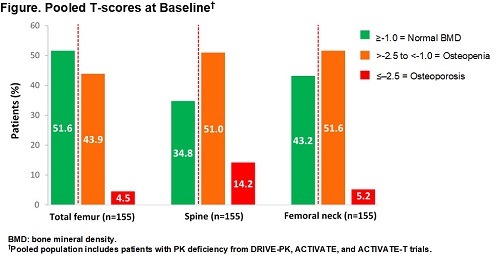
Of 159 pts evaluated (DRIVE-PK, n=52; ACTIVATE, n=80; ACTIVATE-T, n=27), median age was 34 yrs (range, 18–78) and majority were female (n=88; 55.3%). Of 155 pts who had baseline T-scores for total femur, spine, and femoral neck, 38 (24.5%) had a T-score of ≥–1.0 at all locations, indicating normal BMD; 91 (58.7%) had a T-score of >–2.5 to <–1.0 at 1 or more locations, indicating osteopenia; and 26 (16.8%) had a T-score of ≤–2.5 at 1 or more locations, indicating osteoporosis. The proportion of pts in each T-score range for each of the 3 locations is shown in the Figure. In contrast to the DXA scan findings, only 28 (17.6%) pts had a known medical history of osteopenia and 23 (14.5%) had a known medical history of osteoporosis. Taking together DXA scan results and medical history for all 159 pts, 85 (53.5%) had osteopenia and 33 (20.8%) had osteoporosis. Median age for pts with either osteopenia or osteoporosis (n=118) was 36 yrs (range, 18–78). Of these, 20 pts (16.9%) were regularly transfused and 98 pts (83.1%) were not regularly transfused.
Conclusion
In this large cohort, universal DXA scanning revealed that over three-quarters of adults with PK deficiency had osteopenia or osteoporosis, irrespective of transfusion requirements. Given the young median age of the cohort (34 yrs), these findings have considerable significance and implications for the screening and care of pts with PK deficiency throughout their adult lives. Early monitoring of these pts with DXA scans in order to ensure a prompt diagnosis of bone density abnormalities and indicated treatment may be warranted.
Keyword(s): AG-348, Bone mineral density, Osteoporosis, Pyruvate kinase deficiency
Abstract: EP692
Type: E-Poster Presentation
Session title: Enzymopathies, membranopathies and other anemias
Background
Hereditary pyruvate kinase (PK) deficiency results in lifelong hemolytic anemia and several significant comorbidities, the epidemiology of which are not well characterized. Among these is reduced bone mineral density (BMD), which can result in premature osteopenia, osteoporosis, and fractures.
Aims
To better characterize the bone density abnormalities in patients (pts) with PK deficiency, this study evaluated pooled pre-treatment baseline data from 3 clinical trials involving pts with PK deficiency investigating mitapivat (AG-348), an allosteric activator of PK: DRIVE-PK (NCT02476916), ACTIVATE (NCT03548220), and ACTIVATE-T (NCT03559699). This is the first large PK deficiency cohort in which dual-energy x-ray absorptiometry (DXA) scores were systematically and consistently assessed.
Methods
DRIVE-PK is a completed phase 2, global, randomized, open-label study. ACTIVATE is an ongoing phase 3, global, randomized, double-blind, placebo-controlled study. ACTIVATE-T is an ongoing phase 3, global, open-label, single-arm study. In all 3 studies, pts ≥18 years (yrs) of age with a confirmed diagnosis of PK deficiency were eligible to participate. Pts were eligible to participate in DRIVE-PK and in ACTIVATE if they were not regularly transfused (DRIVE-PK: ≤3 units of red blood cells in the prior 12 months [mos]; no transfusions in the prior 4 mos; ACTIVATE: ≤4 transfusion episodes in the previous yr; no transfusions in the prior 3 mos) and in ACTIVATE-T if they were regularly transfused (≥6 transfusion episodes in the previous yr). BMD was measured using DXA at baseline; scans were obtained locally for all 3 studies. Scans were interpreted locally for DRIVE-PK and centrally for ACTIVATE and ACTIVATE-T. Osteopenia and osteoporosis were identified on DXA according to standard definitions, and prevalence of each was compared to prevalence ascertained via medical history.
Results
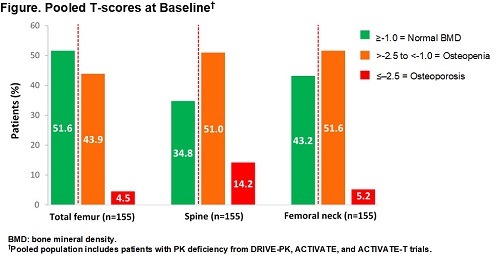
Of 159 pts evaluated (DRIVE-PK, n=52; ACTIVATE, n=80; ACTIVATE-T, n=27), median age was 34 yrs (range, 18–78) and majority were female (n=88; 55.3%). Of 155 pts who had baseline T-scores for total femur, spine, and femoral neck, 38 (24.5%) had a T-score of ≥–1.0 at all locations, indicating normal BMD; 91 (58.7%) had a T-score of >–2.5 to <–1.0 at 1 or more locations, indicating osteopenia; and 26 (16.8%) had a T-score of ≤–2.5 at 1 or more locations, indicating osteoporosis. The proportion of pts in each T-score range for each of the 3 locations is shown in the Figure. In contrast to the DXA scan findings, only 28 (17.6%) pts had a known medical history of osteopenia and 23 (14.5%) had a known medical history of osteoporosis. Taking together DXA scan results and medical history for all 159 pts, 85 (53.5%) had osteopenia and 33 (20.8%) had osteoporosis. Median age for pts with either osteopenia or osteoporosis (n=118) was 36 yrs (range, 18–78). Of these, 20 pts (16.9%) were regularly transfused and 98 pts (83.1%) were not regularly transfused.
Conclusion
In this large cohort, universal DXA scanning revealed that over three-quarters of adults with PK deficiency had osteopenia or osteoporosis, irrespective of transfusion requirements. Given the young median age of the cohort (34 yrs), these findings have considerable significance and implications for the screening and care of pts with PK deficiency throughout their adult lives. Early monitoring of these pts with DXA scans in order to ensure a prompt diagnosis of bone density abnormalities and indicated treatment may be warranted.
Keyword(s): AG-348, Bone mineral density, Osteoporosis, Pyruvate kinase deficiency


