
Contributions
Abstract: EP690
Type: E-Poster Presentation
Session title: Enzymopathies, membranopathies and other anemias
Background
Warm autoimmune haemolytic anaemia (wAIHA) is an acquired blood disorder characterized by antibodies directed against own RBCs. wAIHA is either primary or secondary due to cancers or other diseases. The presence of an underlying disease in wAIHA is associated with an overall reduced prognosis, compared with primary wAIHA. The association between wAIHA and some cancers, especially B-cell malignancies, have been established, but accurate risks are missing. To our knowledge, no studies have investigated the cumulative incidence of cancer following diagnosis of primary or secondary wAIHA.
Aims
The aim of this study is to evaluate the prevalence of any cancer amongst patients with wAIHA at time of diagnosis, compared with the general population, and whether patients with wAIHA have a higher incidence of cancer after wAIHA-diagnosis.
Methods
Patients with wAHIA diagnosed 1980-2016 were identified in the nationwide Danish Haemolysis Cohort. Each patient was age-sex-matched with up to 50 comparisons from the general population without haemolysis. Patients and comparisons were followed from index date, corresponding to date of wAIHA diagnosis or an assigned matched date for comparisons. We identified incident and prevalent cancer diagnoses using the Danish Cancer Registry. Patients and comparisons were followed until a cancer diagnosis, death, emigration or end of study, whichever came first. Any registered cancer diagnosis before index-date + 30 days were considered prevalent, thereafter, all cancer diagnoses were defined as incident cancer diagnosis. We present cumulative incidences (CIs) of cancer diagnoses after one year, five years, and ten years.
Results
We identified 2,700 patients with wAIHA and 133,730 sex and age-matched comparisons. Out of the 2,700 patients with wAIHA, 1,589 (58.9%) were primary wAIHA, and 1,111 (41.1%) patients were secondary wAIHA due to defined underlying diseases – most frequently haematological cancers. Women accounted for 56% of patients, and this uneven sex distribution were most prominent in primary wAIHA. Median age was 58.8 years for patients with primary wAIHA and 68.2 years for secondary wAIHA patients. The mean age at death for the patients diagnosed with primary wAIHA was 77.6 years, 75.0 years for patients diagnosed with secondary wAIHA, and 83.9 and 83.8 years in the respective comparison groups.
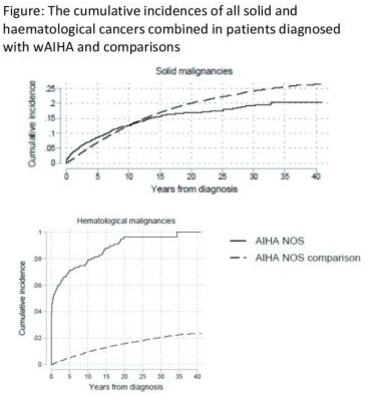
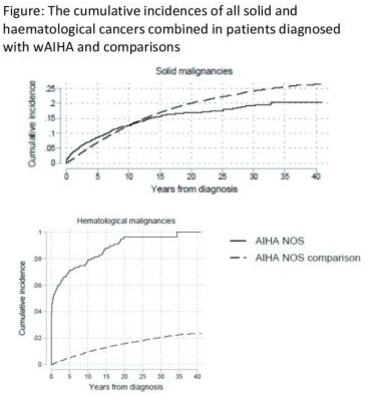
The CI of haematological cancer was higher for patients diagnosed with wAIHA vs. general population comparisons (Figure). For all haematological malignancies, except multiple myeloma, the CI remained higher in wAIHA vs. comparisons. For solid cancer the CI was higher the first 10 years following wAIHA diagnosis vs. comparisons, after time point incidences equalized (Figure).
Conclusion
Patients diagnosed with wAIHA have a higher risk of developing malignancies after the wAIHA diagnosis. The increased risk for subsequent cancer development after wAIHA-diagnosis is most prominent for haematological malignancies.
Keyword(s): Autoimmune hemolytic anemia (AIHA), Cancer, Hematological malignancy, Solid tumor
Abstract: EP690
Type: E-Poster Presentation
Session title: Enzymopathies, membranopathies and other anemias
Background
Warm autoimmune haemolytic anaemia (wAIHA) is an acquired blood disorder characterized by antibodies directed against own RBCs. wAIHA is either primary or secondary due to cancers or other diseases. The presence of an underlying disease in wAIHA is associated with an overall reduced prognosis, compared with primary wAIHA. The association between wAIHA and some cancers, especially B-cell malignancies, have been established, but accurate risks are missing. To our knowledge, no studies have investigated the cumulative incidence of cancer following diagnosis of primary or secondary wAIHA.
Aims
The aim of this study is to evaluate the prevalence of any cancer amongst patients with wAIHA at time of diagnosis, compared with the general population, and whether patients with wAIHA have a higher incidence of cancer after wAIHA-diagnosis.
Methods
Patients with wAHIA diagnosed 1980-2016 were identified in the nationwide Danish Haemolysis Cohort. Each patient was age-sex-matched with up to 50 comparisons from the general population without haemolysis. Patients and comparisons were followed from index date, corresponding to date of wAIHA diagnosis or an assigned matched date for comparisons. We identified incident and prevalent cancer diagnoses using the Danish Cancer Registry. Patients and comparisons were followed until a cancer diagnosis, death, emigration or end of study, whichever came first. Any registered cancer diagnosis before index-date + 30 days were considered prevalent, thereafter, all cancer diagnoses were defined as incident cancer diagnosis. We present cumulative incidences (CIs) of cancer diagnoses after one year, five years, and ten years.
Results
We identified 2,700 patients with wAIHA and 133,730 sex and age-matched comparisons. Out of the 2,700 patients with wAIHA, 1,589 (58.9%) were primary wAIHA, and 1,111 (41.1%) patients were secondary wAIHA due to defined underlying diseases – most frequently haematological cancers. Women accounted for 56% of patients, and this uneven sex distribution were most prominent in primary wAIHA. Median age was 58.8 years for patients with primary wAIHA and 68.2 years for secondary wAIHA patients. The mean age at death for the patients diagnosed with primary wAIHA was 77.6 years, 75.0 years for patients diagnosed with secondary wAIHA, and 83.9 and 83.8 years in the respective comparison groups.
The CI of haematological cancer was higher for patients diagnosed with wAIHA vs. general population comparisons (Figure). For all haematological malignancies, except multiple myeloma, the CI remained higher in wAIHA vs. comparisons. For solid cancer the CI was higher the first 10 years following wAIHA diagnosis vs. comparisons, after time point incidences equalized (Figure).
Conclusion
Patients diagnosed with wAIHA have a higher risk of developing malignancies after the wAIHA diagnosis. The increased risk for subsequent cancer development after wAIHA-diagnosis is most prominent for haematological malignancies.
Keyword(s): Autoimmune hemolytic anemia (AIHA), Cancer, Hematological malignancy, Solid tumor


