
Contributions
Abstract: EP680
Type: E-Poster Presentation
Session title: Chronic myeloid leukemia - Clinical
Background
Withdrawal syndrome (WS) - a musculoskeletal pain after discontinuation of tyrosine kinase inhibitors (TKI) in patients (pts) with chronic myeloid leukemia (CML) - was described in the treatment-free remission (TFR) studies with a weighted mean incidence of 27% [Chen et al, Front Oncol., 2019]. The pathophysiological mechanisms of WS and predisposing factors have not been well established.
Aims
To characterize the outcomes of WS and evaluate factors associated with WS in a large cohort of CML pts who discontinued TKI therapy.
Methods
WS was evaluated in prospective pts group (PG, n=109) and in retrospective group (RG, n=74). The key inclusion criteria: CML chronic phase, any TKI therapy ≥ 3 years, deep molecular response (DMR) duration ≥2 years in PG and ≥1 year in RG. DMR was defined as at least MR4 (BCR-ABL ≤ 0,01% IS). TKI were restarted in both groups in case of major MR (MMR, BCR-ABL>0,1% IS) loss. In 34 pregnant pts (24 and 10 in RG and PG accordingly) TKI were restarted in case of MR2 (BCR-ABL>1%) loss.
WS was defined as a musculoskeletal pain newly observed after TKI cessation or as a worsening of previously observed symptoms in pts with medical history of locomotion system diseases. WS was registered In PG every month (mo) during first 6 mo after TKI cessation, every 2 mo from 6 to 12 mo and every 3 mo thereafter. The data in RG were collected according to medical records.
Age, gender, Sokal score, duration and the type of TKI therapy, presence of locomotion system diseases and pregnancy were evaluated in pts with and without WS. Comparison was done with Mann–Whitney U-test and Chi-squared test. The survival without MMR loss was evaluated by Kaplan-Meier method.
Results
Меdian (Me) time of observation was 33 mo (range 1-136). MMR loss free survival at 36 mo was 49% and 43% in PG and RG respectively (p=0,96).
WS was observed in 49(27%) of 183 pts: 41(38%) in PG and 8(11%) in RG. WS was presented as arthralgia, myalgia, ossalgia or combination of symptoms in 37(76%), 17(35%), 4(8%) and 35(71%) pts. Newly observed and worsening symptoms were in 35(71%) and 14(29%) pts respectively. Me time to WS appearance was 2 mo (range 1-7). Ме duration of WS was 5 mo (range 1-35). WS grade 1-2 was in 45(92%) pts, grade 3 in 4(8%) pts.
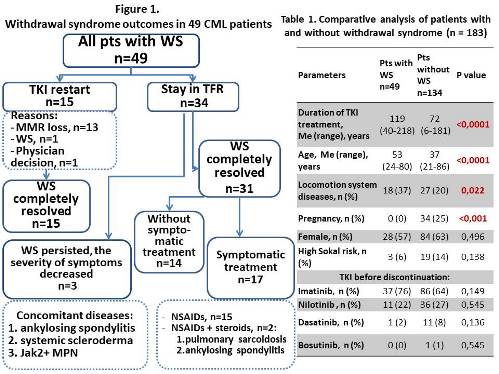
TKI therapy was resumed in 15(31%) of 49 pts with WS: in 13 pts with MMR loss, in 1 pt with 3rd grade WS symptoms and in 1 pt due to physician decision. WS was resolved in all 15 pts at 1-3 mo after TKI restart.
Thirty-four (69%) pts with WS remained in TFR. WS completely resolved in 31 and gradually decreased up to 1st grade in 3 pts at the time of analysis.
WS was resolved spontaneously or with nonsteroidal anti-inflammatory drugs in 14(45%) and 17(55%) pts accordingly. Two of 17 pts also received glucocorticoids. The outcomes of WS are presented on figure 1.
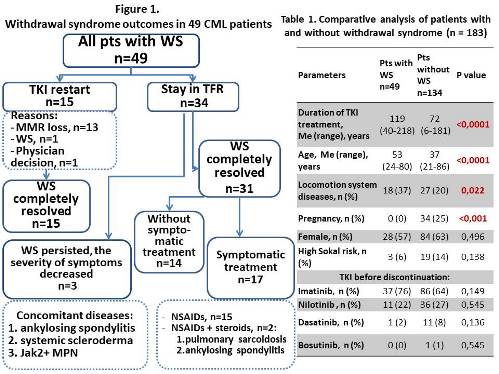
An older age (p<0,0001), longer duration of TKI therapy (p<0,0001) and the presence of locomotion system diseases (p=0,022) were observed in pts with WS (table 1). The development of WS was not registered in any of pregnant pts (р<0,001).
Conclusion
The rate of WS in the large CML cohort was 27%. We evaluate a higher WS incidence in PG compared to RG (38% vs 11%). The differences may be cause by methods of data collection: prospective observation probably allowed to more accurately identifying the presence of WS. On the other hand, there were more pregnant pts in RG, and we found for the first time that WS doesn’t develop in pts with pregnancy. A longer period of TKI exposure, older age and the history of locomotion system diseases were associated with the development of the WS.
Keyword(s): Chronic myeloid leukemia, Treatment-free remission, Tyrosine kinase inhibitor
Abstract: EP680
Type: E-Poster Presentation
Session title: Chronic myeloid leukemia - Clinical
Background
Withdrawal syndrome (WS) - a musculoskeletal pain after discontinuation of tyrosine kinase inhibitors (TKI) in patients (pts) with chronic myeloid leukemia (CML) - was described in the treatment-free remission (TFR) studies with a weighted mean incidence of 27% [Chen et al, Front Oncol., 2019]. The pathophysiological mechanisms of WS and predisposing factors have not been well established.
Aims
To characterize the outcomes of WS and evaluate factors associated with WS in a large cohort of CML pts who discontinued TKI therapy.
Methods
WS was evaluated in prospective pts group (PG, n=109) and in retrospective group (RG, n=74). The key inclusion criteria: CML chronic phase, any TKI therapy ≥ 3 years, deep molecular response (DMR) duration ≥2 years in PG and ≥1 year in RG. DMR was defined as at least MR4 (BCR-ABL ≤ 0,01% IS). TKI were restarted in both groups in case of major MR (MMR, BCR-ABL>0,1% IS) loss. In 34 pregnant pts (24 and 10 in RG and PG accordingly) TKI were restarted in case of MR2 (BCR-ABL>1%) loss.
WS was defined as a musculoskeletal pain newly observed after TKI cessation or as a worsening of previously observed symptoms in pts with medical history of locomotion system diseases. WS was registered In PG every month (mo) during first 6 mo after TKI cessation, every 2 mo from 6 to 12 mo and every 3 mo thereafter. The data in RG were collected according to medical records.
Age, gender, Sokal score, duration and the type of TKI therapy, presence of locomotion system diseases and pregnancy were evaluated in pts with and without WS. Comparison was done with Mann–Whitney U-test and Chi-squared test. The survival without MMR loss was evaluated by Kaplan-Meier method.
Results
Меdian (Me) time of observation was 33 mo (range 1-136). MMR loss free survival at 36 mo was 49% and 43% in PG and RG respectively (p=0,96).
WS was observed in 49(27%) of 183 pts: 41(38%) in PG and 8(11%) in RG. WS was presented as arthralgia, myalgia, ossalgia or combination of symptoms in 37(76%), 17(35%), 4(8%) and 35(71%) pts. Newly observed and worsening symptoms were in 35(71%) and 14(29%) pts respectively. Me time to WS appearance was 2 mo (range 1-7). Ме duration of WS was 5 mo (range 1-35). WS grade 1-2 was in 45(92%) pts, grade 3 in 4(8%) pts.
TKI therapy was resumed in 15(31%) of 49 pts with WS: in 13 pts with MMR loss, in 1 pt with 3rd grade WS symptoms and in 1 pt due to physician decision. WS was resolved in all 15 pts at 1-3 mo after TKI restart.
Thirty-four (69%) pts with WS remained in TFR. WS completely resolved in 31 and gradually decreased up to 1st grade in 3 pts at the time of analysis.
WS was resolved spontaneously or with nonsteroidal anti-inflammatory drugs in 14(45%) and 17(55%) pts accordingly. Two of 17 pts also received glucocorticoids. The outcomes of WS are presented on figure 1.
An older age (p<0,0001), longer duration of TKI therapy (p<0,0001) and the presence of locomotion system diseases (p=0,022) were observed in pts with WS (table 1). The development of WS was not registered in any of pregnant pts (р<0,001).
Conclusion
The rate of WS in the large CML cohort was 27%. We evaluate a higher WS incidence in PG compared to RG (38% vs 11%). The differences may be cause by methods of data collection: prospective observation probably allowed to more accurately identifying the presence of WS. On the other hand, there were more pregnant pts in RG, and we found for the first time that WS doesn’t develop in pts with pregnancy. A longer period of TKI exposure, older age and the history of locomotion system diseases were associated with the development of the WS.
Keyword(s): Chronic myeloid leukemia, Treatment-free remission, Tyrosine kinase inhibitor


