
Contributions
Abstract: EP677
Type: E-Poster Presentation
Session title: Chronic myeloid leukemia - Clinical
Background
Tyrosine kinase inhibitors (TKIs) have dramatically improved the standard of care for patients (pts) with chronic myeloid leukemia in chronic phase (CML-CP). In the 5-y follow-up of the phase 3 DASISION study (NCT00481247), dasatinib (DAS) was associated with faster and deeper molecular responses than imatinib (IM) as first-line (1L) therapy for CML-CP. The NCCN guidelines recommend considering multiple factors independent of risk score when selecting TKI therapy, including the presence of comorbidities. Over 50% of pts with CML-CP have ≥1 comorbidity at diagnosis; as such, comorbidities may influence 1L treatment (Tx) choice for most pts.
Aims
Investigate the effect of comorbidities on response outcomes with DAS vs IM via an exploratory post hoc analysis of DASISION at 5-y follow-up.
Methods
DASISION was a multinational, open-label, phase 3 trial assessing DAS vs IM for newly diagnosed CML-CP. Pts were randomized to receive 100 mg DAS (n=259) or 400 mg IM (n=260) QD. Charlson Comorbidity Index (CCI) was retrospectively calculated for each pt at diagnosis. Efficacy and safety data were retrospectively stratified based on CCI score categories 2–4, 5–6, and ≥7 (higher scores indicate higher comorbidity burden). Rates of major molecular response (MMR) and MR4.5 were compared between Tx arms using unstratified Cochran–Mantel–Haenszel tests. Time to MMR and MR4.5 were evaluated using Kaplan–Meier method with HRs based on Cox proportional hazards models and P values from unstratified log-rank tests. CIs for median time to response were calculated using the Brookmeyer and Crowley method. P values are descriptive and unadjusted for multiple comparisons.
Results
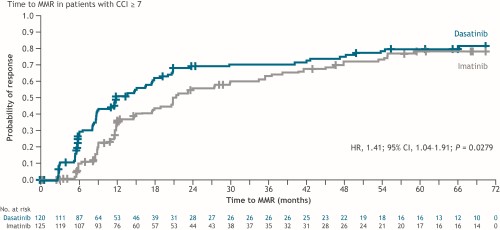
In total, 14 (3%) pts had CCI 2–4 (DAS 7, IM 7), 260 (50%) had CCI 5–6 (DAS 132, IM 128), and 245 (47%) had CCI ≥7 (DAS 120, IM 125). Baseline characteristics were balanced between groups. Dose reductions of DAS and IM occurred in 14% vs 29% (CCI 2–4 group), 23% vs 12% (CCI 5–6 group) and 54% vs 22% (CCI ≥7 group) of pts, respectively. Responses were greater with DAS vs IM in the CCI 2–4 group (MMR: 85.7% vs 57.1%, P=0.2542; MR4.5: 71.4% vs 14.3%, P=0.0374), and were significantly higher in the CCI 5–6 group (MMR: 81.1% vs 64.8%, P=0.0033; MR4.5: 42.4% vs 29.7%, P=0.0329). Median time to MMR in the CCI 5–6 group was significantly shorter with DAS vs IM (15.0 vs 24.0 months; HR,1.64; P=0.0006). In the CCI ≥7 group, response rates were numerically higher (MMR: 70.8% vs 64.0%; MR4.5: 45.0% vs 39.2%) and median time to MMR was significantly shorter with DAS vs IM (12.0 vs 21.4 months; HR, 1.41; P=0.0279; Figure). Rates of grade (gr) 3–4 Tx-related adverse events (TRAEs) were (DAS vs IM): 0% vs 14% (CCI 2–4); 8% vs 9% (CCI 5–6); 24% vs 13% (CCI ≥7). Gr 3–4 TRAEs leading to discontinuation did not occur in the CCI 2–4 group, and were reported with similar frequency with DAS and IM in CCI 5–6 and ≥7 groups. No deaths occurred in the CCI 2–4 group; a similar percentage of pts treated with DAS and IM died in the CCI 5–6 and ≥7 groups.
Conclusion
In this exploratory post hoc analysis, DAS was effective in all CCI groups, in line with previous findings, suggesting that comorbidities do not negatively affect TKI activity. Response rates were significantly higher with DAS than IM in pts with CCI 5–6, but comparable between Txs in pts with CCI ≥7. Time to response was significantly faster with DAS than IM in both the CCI 5–6 and ≥7 groups, while the frequency of gr 3–4 TRAEs leading to discontinuation was similar between Txs. These findings highlight the benefit of 1L Tx with DAS in pts with CML-CP and a high comorbidity burden.
Keyword(s): Chronic myeloid leukemia, Comorbidities, Molecular response, Tyrosine kinase inhibitor
Abstract: EP677
Type: E-Poster Presentation
Session title: Chronic myeloid leukemia - Clinical
Background
Tyrosine kinase inhibitors (TKIs) have dramatically improved the standard of care for patients (pts) with chronic myeloid leukemia in chronic phase (CML-CP). In the 5-y follow-up of the phase 3 DASISION study (NCT00481247), dasatinib (DAS) was associated with faster and deeper molecular responses than imatinib (IM) as first-line (1L) therapy for CML-CP. The NCCN guidelines recommend considering multiple factors independent of risk score when selecting TKI therapy, including the presence of comorbidities. Over 50% of pts with CML-CP have ≥1 comorbidity at diagnosis; as such, comorbidities may influence 1L treatment (Tx) choice for most pts.
Aims
Investigate the effect of comorbidities on response outcomes with DAS vs IM via an exploratory post hoc analysis of DASISION at 5-y follow-up.
Methods
DASISION was a multinational, open-label, phase 3 trial assessing DAS vs IM for newly diagnosed CML-CP. Pts were randomized to receive 100 mg DAS (n=259) or 400 mg IM (n=260) QD. Charlson Comorbidity Index (CCI) was retrospectively calculated for each pt at diagnosis. Efficacy and safety data were retrospectively stratified based on CCI score categories 2–4, 5–6, and ≥7 (higher scores indicate higher comorbidity burden). Rates of major molecular response (MMR) and MR4.5 were compared between Tx arms using unstratified Cochran–Mantel–Haenszel tests. Time to MMR and MR4.5 were evaluated using Kaplan–Meier method with HRs based on Cox proportional hazards models and P values from unstratified log-rank tests. CIs for median time to response were calculated using the Brookmeyer and Crowley method. P values are descriptive and unadjusted for multiple comparisons.
Results
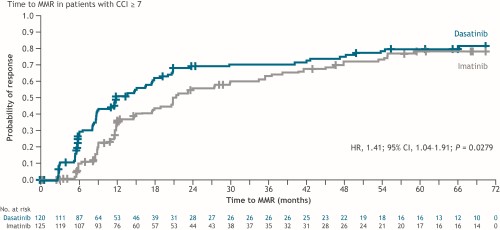
In total, 14 (3%) pts had CCI 2–4 (DAS 7, IM 7), 260 (50%) had CCI 5–6 (DAS 132, IM 128), and 245 (47%) had CCI ≥7 (DAS 120, IM 125). Baseline characteristics were balanced between groups. Dose reductions of DAS and IM occurred in 14% vs 29% (CCI 2–4 group), 23% vs 12% (CCI 5–6 group) and 54% vs 22% (CCI ≥7 group) of pts, respectively. Responses were greater with DAS vs IM in the CCI 2–4 group (MMR: 85.7% vs 57.1%, P=0.2542; MR4.5: 71.4% vs 14.3%, P=0.0374), and were significantly higher in the CCI 5–6 group (MMR: 81.1% vs 64.8%, P=0.0033; MR4.5: 42.4% vs 29.7%, P=0.0329). Median time to MMR in the CCI 5–6 group was significantly shorter with DAS vs IM (15.0 vs 24.0 months; HR,1.64; P=0.0006). In the CCI ≥7 group, response rates were numerically higher (MMR: 70.8% vs 64.0%; MR4.5: 45.0% vs 39.2%) and median time to MMR was significantly shorter with DAS vs IM (12.0 vs 21.4 months; HR, 1.41; P=0.0279; Figure). Rates of grade (gr) 3–4 Tx-related adverse events (TRAEs) were (DAS vs IM): 0% vs 14% (CCI 2–4); 8% vs 9% (CCI 5–6); 24% vs 13% (CCI ≥7). Gr 3–4 TRAEs leading to discontinuation did not occur in the CCI 2–4 group, and were reported with similar frequency with DAS and IM in CCI 5–6 and ≥7 groups. No deaths occurred in the CCI 2–4 group; a similar percentage of pts treated with DAS and IM died in the CCI 5–6 and ≥7 groups.
Conclusion
In this exploratory post hoc analysis, DAS was effective in all CCI groups, in line with previous findings, suggesting that comorbidities do not negatively affect TKI activity. Response rates were significantly higher with DAS than IM in pts with CCI 5–6, but comparable between Txs in pts with CCI ≥7. Time to response was significantly faster with DAS than IM in both the CCI 5–6 and ≥7 groups, while the frequency of gr 3–4 TRAEs leading to discontinuation was similar between Txs. These findings highlight the benefit of 1L Tx with DAS in pts with CML-CP and a high comorbidity burden.
Keyword(s): Chronic myeloid leukemia, Comorbidities, Molecular response, Tyrosine kinase inhibitor


