
Contributions
Abstract: EP675
Type: E-Poster Presentation
Session title: Chronic myeloid leukemia - Clinical
Background
Creatine kinase (CK) elevation is seen with tyrosine kinase inhibitor (TKI) treatment for Chronic Myeloid Leukemia (CML). Its correlation with musculoskeletal (MSK) symptoms and treatment outcomes in not well studied.
Aims
To measure the association CK elevation with overall (OS) and event-free survival (EFS) in patients with CML.
Methods
Retrospective, single-centre study on all newly diagnosed chronic phase CML patients from 2001 to 2017 seen and followed by senior author on study at Princess Margaret Cancer Centre, Toronto, Canada. Primary exposure was CK elevation after initiation of first line TKI, defined as two CK values above baseline within any 6 months period. Clinical variables were age, sex, cardiovascular risk factors (smoking, hypertension, diabetes mellitus, and hypercholesterolemia), sokal index and use of second line TKI. Primary outcome was OS, and secondary outcomes were EFS and cumulative incidence of CK elevation. The effect of covariates was measured as hazard ratio (HR, 95% CI) using cox proportional hazard models and compared with log rank test.
Results
Total 283 newly diagnosed CML patients were included. The median age was 49.8 years (18.0-82.0), 54.1% were male. The median follow-up was 8.8 years (IQR 4.4-12.7). The median baseline CK was 100 IU/L (10.0-1490). First line TKI were imatinib (78.1%), followed by dasatinib (11.0%), nilotinib (8.1%) and bosutinib (2.8%). 203 patients (72%) had CK elevation [76% (169/221) on imatinib, 54% (34/62) on second generation TKI (SG-TKI)]. The median time to CK elevation with imatinib was 1.0 years (IQR 0.8-1.3) compared to 1.2 years, (IQR 0.5-3.7) with SG-TKI. There was no difference in the cumulative incidence of CK elevation between imatinib (HR 0.92, 0.64-1.35) and SG-TKI. There was no difference in grade of CK elevation between different TKIs (anova, p=0.57). CK levels of patients with MSK symptoms were higher compared to those without (t-test, p=0.02). 3 patients on imatinib had rhabdomyolysis.
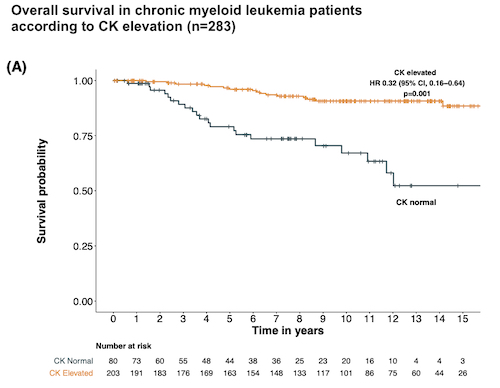
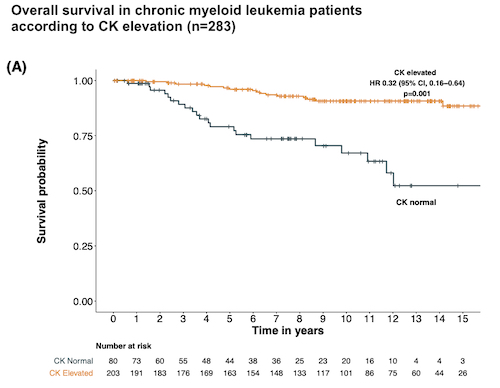
38 patients (13.4%) died during follow-up. Using CK elevation as time-dependent covariate, the Kaplan–Meier survival analysis showed that patients with CK elevation had a lower probability of death (7.8%, 16/203) compared to those with normal CK (27.5%, 22/80) (p<0.001). In multivariable Cox regression, the impact of CK elevation on OS remained unchanged: adjusted HRs for OS were 0.31 (0.16–0.60) for CK elevation; 3.39 (1.67–6.84) for intermediate sokal and 5.11 (1.95-13.4) for high sokal risk.
116 patients (41%) were considered for secondary outcome-EFS [98 discontinued treatment-46 suboptimal response or progression, 52-toxicity; 18 patients died without treatment related event]. Using CK elevation as time-dependent covariate, Kaplan–Meier survival function showed that patients with CK elevation had a lower probability of an event compared to those without CK elevation (p=0.003). In multivariable Cox regression, the impact of CK elevation on EFS remained unchanged: adjusted HR for EFS were 0.51 (0.33–0.79) for CK elevation. Other significant variables were intermediate and high sokal risk, SG-TKI (better EFS); higher comorbidities (worse EFS).
Conclusion
The cumulative incidence of CK elevation in CML patients on TKI is 72% with no difference between imatinib and SG- TKI. CK levels correlated with MSK symptoms but rhabdomyolysis was rare. CK elevation independently predicted better OS and EFS. These results inform clinicians on not discontinuing TKI based on laboratory elevation of CK alone.
Keyword(s):
Abstract: EP675
Type: E-Poster Presentation
Session title: Chronic myeloid leukemia - Clinical
Background
Creatine kinase (CK) elevation is seen with tyrosine kinase inhibitor (TKI) treatment for Chronic Myeloid Leukemia (CML). Its correlation with musculoskeletal (MSK) symptoms and treatment outcomes in not well studied.
Aims
To measure the association CK elevation with overall (OS) and event-free survival (EFS) in patients with CML.
Methods
Retrospective, single-centre study on all newly diagnosed chronic phase CML patients from 2001 to 2017 seen and followed by senior author on study at Princess Margaret Cancer Centre, Toronto, Canada. Primary exposure was CK elevation after initiation of first line TKI, defined as two CK values above baseline within any 6 months period. Clinical variables were age, sex, cardiovascular risk factors (smoking, hypertension, diabetes mellitus, and hypercholesterolemia), sokal index and use of second line TKI. Primary outcome was OS, and secondary outcomes were EFS and cumulative incidence of CK elevation. The effect of covariates was measured as hazard ratio (HR, 95% CI) using cox proportional hazard models and compared with log rank test.
Results
Total 283 newly diagnosed CML patients were included. The median age was 49.8 years (18.0-82.0), 54.1% were male. The median follow-up was 8.8 years (IQR 4.4-12.7). The median baseline CK was 100 IU/L (10.0-1490). First line TKI were imatinib (78.1%), followed by dasatinib (11.0%), nilotinib (8.1%) and bosutinib (2.8%). 203 patients (72%) had CK elevation [76% (169/221) on imatinib, 54% (34/62) on second generation TKI (SG-TKI)]. The median time to CK elevation with imatinib was 1.0 years (IQR 0.8-1.3) compared to 1.2 years, (IQR 0.5-3.7) with SG-TKI. There was no difference in the cumulative incidence of CK elevation between imatinib (HR 0.92, 0.64-1.35) and SG-TKI. There was no difference in grade of CK elevation between different TKIs (anova, p=0.57). CK levels of patients with MSK symptoms were higher compared to those without (t-test, p=0.02). 3 patients on imatinib had rhabdomyolysis.
38 patients (13.4%) died during follow-up. Using CK elevation as time-dependent covariate, the Kaplan–Meier survival analysis showed that patients with CK elevation had a lower probability of death (7.8%, 16/203) compared to those with normal CK (27.5%, 22/80) (p<0.001). In multivariable Cox regression, the impact of CK elevation on OS remained unchanged: adjusted HRs for OS were 0.31 (0.16–0.60) for CK elevation; 3.39 (1.67–6.84) for intermediate sokal and 5.11 (1.95-13.4) for high sokal risk.
116 patients (41%) were considered for secondary outcome-EFS [98 discontinued treatment-46 suboptimal response or progression, 52-toxicity; 18 patients died without treatment related event]. Using CK elevation as time-dependent covariate, Kaplan–Meier survival function showed that patients with CK elevation had a lower probability of an event compared to those without CK elevation (p=0.003). In multivariable Cox regression, the impact of CK elevation on EFS remained unchanged: adjusted HR for EFS were 0.51 (0.33–0.79) for CK elevation. Other significant variables were intermediate and high sokal risk, SG-TKI (better EFS); higher comorbidities (worse EFS).
Conclusion
The cumulative incidence of CK elevation in CML patients on TKI is 72% with no difference between imatinib and SG- TKI. CK levels correlated with MSK symptoms but rhabdomyolysis was rare. CK elevation independently predicted better OS and EFS. These results inform clinicians on not discontinuing TKI based on laboratory elevation of CK alone.
Keyword(s):


