
Contributions
Abstract: EP666
Type: E-Poster Presentation
Session title: Chronic myeloid leukemia - Clinical
Background
The negative prognostic impact of high-risk additional cytogenetic abnormalities (HR-ACAs) in chronic myeloid leukemia (CML) is well established. Also, the EUTOS long-term survival score ELTS may be used to identify patients at increased risk for CML-related death during TKI therapy. However, it has not been investigated if HR-ACAs and higher ELTS are related and if a better prognostic prediction may be achieved when combining HR-ACAs and the ELTS.
Aims
The objectives were to assess the relation of HR-ACA with the ELTS at diagnosis and to evaluate the impact of HR-ACA in addition to ELTS on survival in a real-world CML patient population.
Methods
This retrospective analysis was performed using data derived from a real-world population-based registry of 480 Dutch CML patients diagnosed between 2008 and April 2013 (The PHAROS CML Registry combined with HemoBase) with a follow-up until February 2016. HR-ACAs were defined according to the stratification of Hehlmann et al. (Leukemia 2020): +8, +Ph, +19, +21, +17 (or i[17q]), 3q26.2, 11q23, −7/7q− and complex karyotypes (≥3 ACAs) in Ph-positive cells. Loss of the Y chromosome and other ACAs were classified as low-risk ACAs. Overall and progression-free survival (OS and PFS) analyses were performed using the Kaplan Meier method and the log-rank method to test for equality. PFS in chronic phase CML was measured from diagnosis to death or progression to AP/BC; patients in AP/BC at diagnosis were excluded from this analysis.
Results
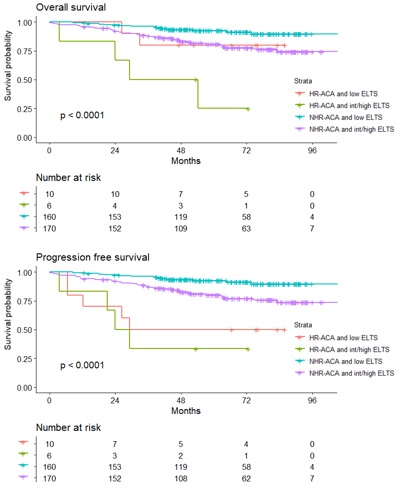
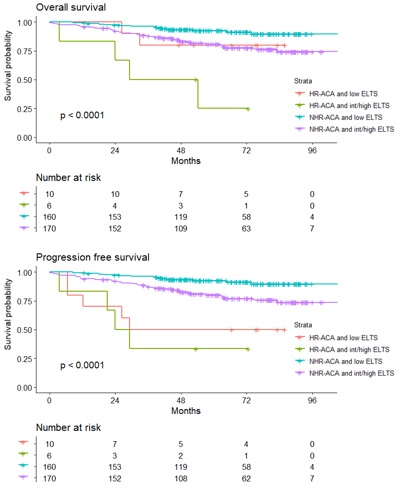
Cytogenetic assessments were available for 415 (86.4%) patients, of whom 20 (4.8%) had HR-ACAs. Trisomy 8 and an additional Ph-chromosome were the most prevalent HR-ACA. HR-ACA had a significant negative prognostic impact on both OS (HR 3.24; 95% CI, 1.61-6.49; p = 0.001) and PFS (HR 4.76; 95% CI, 2.44-9.35; p < 0.001). Low-risk ACA in Ph-positive cells or clonal cytogenetic aberrations in Ph-negative cells (CCA/Ph-) had no prognostic impact. No significant difference in Sokal-score or ELTS was found in patients with versus without HR-ACA (p = 0.573 and p = 0.831). HR-ACA was confirmed as an independent prognostic factor in a cox-regression multivariable analysis with the ELTS at diagnosis and type of first-line TKI as covariables. In our subgroup analysis, patients with both HR-ACAs and an intermediate to high ELTS at diagnosis had a markedly reduced OS compared to patients without HR-ACA or with a low ELTS (figure: plot 1). In the PFS analysis, both HR-ACA subgroups had a significantly reduced survival probability compared to patients without HR-ACA (figure: plot 2).
Conclusion
These results confirm the negative prognostic impact of HR-ACA on newly diagnosed CML patients and support its implementation as an independent risk-variable in a new prognostic model, including both the presence HR-ACA and the ELTS at diagnosis. Furthermore, they provide a first validation of the ACA risk stratification proposed by Hehlmann et al. since our survival analysis clearly distinguishes HR-ACAs from low-risk ACA or CCA/Ph-. Patients with HR-ACA at diagnosis or int/high ELTS, and especially when in combination, may benefit from a more aggressive treatment approach with upfront 2GTKI, a more stringent response monitoring and an early consideration of allogeneic stem cell transplantation in case of inadequate treatment responses.
Keyword(s): Chronic myeloid leukemia, Cytogenetic abnormalities, Survival prediction
Abstract: EP666
Type: E-Poster Presentation
Session title: Chronic myeloid leukemia - Clinical
Background
The negative prognostic impact of high-risk additional cytogenetic abnormalities (HR-ACAs) in chronic myeloid leukemia (CML) is well established. Also, the EUTOS long-term survival score ELTS may be used to identify patients at increased risk for CML-related death during TKI therapy. However, it has not been investigated if HR-ACAs and higher ELTS are related and if a better prognostic prediction may be achieved when combining HR-ACAs and the ELTS.
Aims
The objectives were to assess the relation of HR-ACA with the ELTS at diagnosis and to evaluate the impact of HR-ACA in addition to ELTS on survival in a real-world CML patient population.
Methods
This retrospective analysis was performed using data derived from a real-world population-based registry of 480 Dutch CML patients diagnosed between 2008 and April 2013 (The PHAROS CML Registry combined with HemoBase) with a follow-up until February 2016. HR-ACAs were defined according to the stratification of Hehlmann et al. (Leukemia 2020): +8, +Ph, +19, +21, +17 (or i[17q]), 3q26.2, 11q23, −7/7q− and complex karyotypes (≥3 ACAs) in Ph-positive cells. Loss of the Y chromosome and other ACAs were classified as low-risk ACAs. Overall and progression-free survival (OS and PFS) analyses were performed using the Kaplan Meier method and the log-rank method to test for equality. PFS in chronic phase CML was measured from diagnosis to death or progression to AP/BC; patients in AP/BC at diagnosis were excluded from this analysis.
Results
Cytogenetic assessments were available for 415 (86.4%) patients, of whom 20 (4.8%) had HR-ACAs. Trisomy 8 and an additional Ph-chromosome were the most prevalent HR-ACA. HR-ACA had a significant negative prognostic impact on both OS (HR 3.24; 95% CI, 1.61-6.49; p = 0.001) and PFS (HR 4.76; 95% CI, 2.44-9.35; p < 0.001). Low-risk ACA in Ph-positive cells or clonal cytogenetic aberrations in Ph-negative cells (CCA/Ph-) had no prognostic impact. No significant difference in Sokal-score or ELTS was found in patients with versus without HR-ACA (p = 0.573 and p = 0.831). HR-ACA was confirmed as an independent prognostic factor in a cox-regression multivariable analysis with the ELTS at diagnosis and type of first-line TKI as covariables. In our subgroup analysis, patients with both HR-ACAs and an intermediate to high ELTS at diagnosis had a markedly reduced OS compared to patients without HR-ACA or with a low ELTS (figure: plot 1). In the PFS analysis, both HR-ACA subgroups had a significantly reduced survival probability compared to patients without HR-ACA (figure: plot 2).
Conclusion
These results confirm the negative prognostic impact of HR-ACA on newly diagnosed CML patients and support its implementation as an independent risk-variable in a new prognostic model, including both the presence HR-ACA and the ELTS at diagnosis. Furthermore, they provide a first validation of the ACA risk stratification proposed by Hehlmann et al. since our survival analysis clearly distinguishes HR-ACAs from low-risk ACA or CCA/Ph-. Patients with HR-ACA at diagnosis or int/high ELTS, and especially when in combination, may benefit from a more aggressive treatment approach with upfront 2GTKI, a more stringent response monitoring and an early consideration of allogeneic stem cell transplantation in case of inadequate treatment responses.
Keyword(s): Chronic myeloid leukemia, Cytogenetic abnormalities, Survival prediction


