
Contributions
Abstract: EP570
Type: E-Poster Presentation
Session title: Bleeding disorders (congenital and acquired)
Background
Factor XI (FXI) deficiency (FXIDef) is an otherwise rare bleeding disorder that commonly affects Ashkenazi and Iraqi Jews, with a homozygous prevalence of 1:450, and a heterozygosity rate of 8%. In the general population, however, heterozygosity rate is estimated to be 1%. Pregnancy in these women poses a potential increased bleeding risk during delivery.
Aims
We describe the experience of an Outpatient Hematology Service in New York to which pregnant women with FXIDef are referred. Different genotypes of FXIDef and their impacts on patients’ phenotypes were analyzed.
Methods
We identified 39 patients with FXIDef evaluated by a single provider between October/2016 and February/2020. Diagnosis was established on routine genetic screening during pregnancy. Epidemiological, clinical, and laboratory data were reviewed. Anesthetic modalities and routes of delivery were also extracted from the records. FXI activity (FXIAct) was measured at initial visit, and near term, at approximately gestational week 37. Basic statistical data for relevant parameters were calculated. Comparisons between FXIAct at first visit and near term, and between genotypes, were made with two-sample T-test.
Results
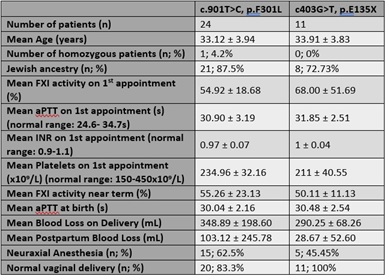
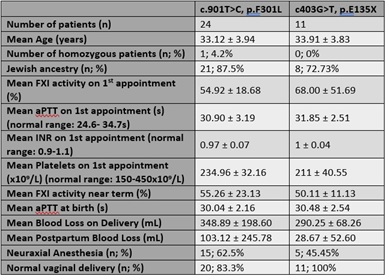
In the sample, 61.54% presented mutation c.901T>C, p.F301L (c.901); 28.20% had mutation c.403G>T, p.E135X (c.403); and 10.26% had 4 different mutations. In the c.901 group, 87.5% showed Jewish ancestry, while 72.73% in the c.403 group presented this ancestry. No statistically significant difference (p=0.43) in FXIAct at first visit was seen between the commonest mutations, also without difference near term (p=0.45). Comparing FXIAct between the first appointment and near term within the c.901 group showed no significant difference (p=0.96), and no difference was noted when comparing the same parameters within the c.403 group (p=0.29). Most patients had a normal vaginal delivery, with no complications recorded, with no need for therapeutic interventions secondary to excessive bleeding. One patient (c.901 group) received a prophylactic intervention before delivery, receiving intravenous tranexamic acid before delivery due to a FIXAct of 42%. Only a single patient from our analysis was homozygous, and she presented mutation c.901. This patient did not receive any special prophylactic or therapeutic interventions before or during delivery. See the attached table for further data.
Conclusion
No significant differences were noted between genotypes in our series. Genotypes correlate with ethnicity, with mutations c.901 and c.403 associated with Jewish ancestry. Comparing our data with other cohorts may allow for broadening of the finding that different genotypes do not affect presentation during pregnancy. Nonetheless, monitoring for FXIDef allows for prophylactic treatment in cases of increased bleeding risk, and it also contributes when deciding the best type of anesthesia for these patients, as neuraxial block is usually contraindicated in cases with FXIAct <40% in our institution. Therefore, genetic tests are valuable for counseling and diagnostic purposes, as well as measuring FXIAct is still relevant in pregnancy. However, as no significant difference in FIXAct was noted between initial visits and near term visits, similar to what has been described in other cohorts, reassessing FXIAct throughout pregnancy may not be necessary. Further studies and continuation of this project will assist in answering this question.
Keyword(s): Factors, Pregnancy
Abstract: EP570
Type: E-Poster Presentation
Session title: Bleeding disorders (congenital and acquired)
Background
Factor XI (FXI) deficiency (FXIDef) is an otherwise rare bleeding disorder that commonly affects Ashkenazi and Iraqi Jews, with a homozygous prevalence of 1:450, and a heterozygosity rate of 8%. In the general population, however, heterozygosity rate is estimated to be 1%. Pregnancy in these women poses a potential increased bleeding risk during delivery.
Aims
We describe the experience of an Outpatient Hematology Service in New York to which pregnant women with FXIDef are referred. Different genotypes of FXIDef and their impacts on patients’ phenotypes were analyzed.
Methods
We identified 39 patients with FXIDef evaluated by a single provider between October/2016 and February/2020. Diagnosis was established on routine genetic screening during pregnancy. Epidemiological, clinical, and laboratory data were reviewed. Anesthetic modalities and routes of delivery were also extracted from the records. FXI activity (FXIAct) was measured at initial visit, and near term, at approximately gestational week 37. Basic statistical data for relevant parameters were calculated. Comparisons between FXIAct at first visit and near term, and between genotypes, were made with two-sample T-test.
Results
In the sample, 61.54% presented mutation c.901T>C, p.F301L (c.901); 28.20% had mutation c.403G>T, p.E135X (c.403); and 10.26% had 4 different mutations. In the c.901 group, 87.5% showed Jewish ancestry, while 72.73% in the c.403 group presented this ancestry. No statistically significant difference (p=0.43) in FXIAct at first visit was seen between the commonest mutations, also without difference near term (p=0.45). Comparing FXIAct between the first appointment and near term within the c.901 group showed no significant difference (p=0.96), and no difference was noted when comparing the same parameters within the c.403 group (p=0.29). Most patients had a normal vaginal delivery, with no complications recorded, with no need for therapeutic interventions secondary to excessive bleeding. One patient (c.901 group) received a prophylactic intervention before delivery, receiving intravenous tranexamic acid before delivery due to a FIXAct of 42%. Only a single patient from our analysis was homozygous, and she presented mutation c.901. This patient did not receive any special prophylactic or therapeutic interventions before or during delivery. See the attached table for further data.
Conclusion
No significant differences were noted between genotypes in our series. Genotypes correlate with ethnicity, with mutations c.901 and c.403 associated with Jewish ancestry. Comparing our data with other cohorts may allow for broadening of the finding that different genotypes do not affect presentation during pregnancy. Nonetheless, monitoring for FXIDef allows for prophylactic treatment in cases of increased bleeding risk, and it also contributes when deciding the best type of anesthesia for these patients, as neuraxial block is usually contraindicated in cases with FXIAct <40% in our institution. Therefore, genetic tests are valuable for counseling and diagnostic purposes, as well as measuring FXIAct is still relevant in pregnancy. However, as no significant difference in FIXAct was noted between initial visits and near term visits, similar to what has been described in other cohorts, reassessing FXIAct throughout pregnancy may not be necessary. Further studies and continuation of this project will assist in answering this question.
Keyword(s): Factors, Pregnancy


