
Contributions
Abstract: EP565
Type: E-Poster Presentation
Session title: Aggressive Non-Hodgkin lymphoma - Clinical
Background
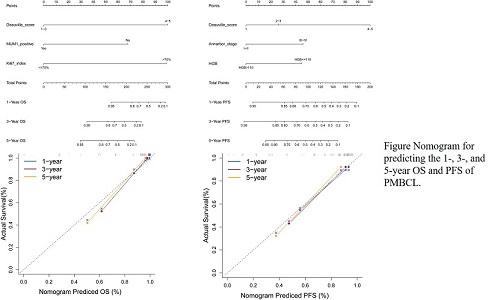
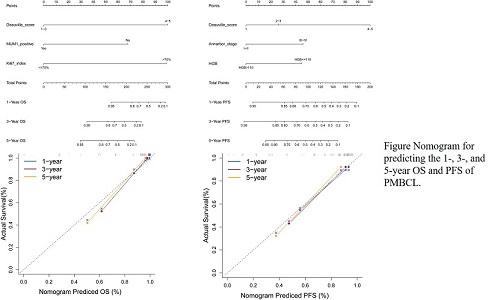
Primary mediastinal large B-cell lymphoma (PMBCL) is rare, and most patients present with large anterior mediastinal tumors that progress rapidly. In PMBCL, the predictive effectiveness of the International Prognostic Index (IPI) is limited by the age composition of the disease and the fact that lesions are usually confined to the mediastinum. This is reflected clinically by the fact that more than half of the patients exhibit lower IPI score. Therefore, a new risk stratification profile is needed to guide the prognostic stratification of PMBCL patients. In addition, the certainty of existing models needs further validation in the era of modern treatments. The nomogram, as a graphical representation of a mathematical model, can be used in clinical practice to combine different information from various features to predict specific outcomes. By combining various important factors, a nomogram can estimate the feasibility of each patient event, such as the likelihood of death or recurrence. Thus, the nomogram has developed into an important tool for predicting clinical outcomes in various types of cancer and can provide physicians with optimal treatment options.
Aims
Our goal was to develop a reliable nomogram to predict overall survival (OS) and progression free survival (PFS) in patients with PMBCL.
Methods
Based on data from Sun Yat-Sen University Cancer Center and the First Hospital of Guangzhou Medical University,116 patients diagnosed with PMBCL were enrolled in this study. Independent prognostic factors were screened by Cox regression analysis. R-coding was used to construct nomograms predicting OS and PFS. Discriminations and corrections of the new model were evaluated using the consistency index (C-index), subject operating characteristic curves (ROC) and calibration curves, and compared with the conventional International Prognostic Index (IPI) using decision curve analysis (DCA) to assess its accuracy and benefit.
Results
Multivariate models showed that post-treatment Deauville score, Ann Arbor staging and hemoglobin level were significantly associated with PFS, while post-treatment Deauville score, MUM1 expression and Ki67 index were significantly associated with OS, and the corresponding nomograms were plotted. In the training cohort, the C-index of the nomogram for PFS and OS was 0.833 and 0.931, respectively. The C-index of the validation cohort was 0.649 and 0.661, respectively. The calibration curves of the nomogram also showed high predictive accuracy. Compared to the IPI scores,the C-index and ROC curves of the Nomogram had better results and also showed better results in the decision curve analysis, yielding better net benefits.
Conclusion
In summary, we have successfully established a valid nomogram for predicting OS and PFS in PMBCL patients, which can help clinicians to select appropriate individualized treatment for their patients.
Keyword(s): Lymphoma, Survival prediction
Abstract: EP565
Type: E-Poster Presentation
Session title: Aggressive Non-Hodgkin lymphoma - Clinical
Background
Primary mediastinal large B-cell lymphoma (PMBCL) is rare, and most patients present with large anterior mediastinal tumors that progress rapidly. In PMBCL, the predictive effectiveness of the International Prognostic Index (IPI) is limited by the age composition of the disease and the fact that lesions are usually confined to the mediastinum. This is reflected clinically by the fact that more than half of the patients exhibit lower IPI score. Therefore, a new risk stratification profile is needed to guide the prognostic stratification of PMBCL patients. In addition, the certainty of existing models needs further validation in the era of modern treatments. The nomogram, as a graphical representation of a mathematical model, can be used in clinical practice to combine different information from various features to predict specific outcomes. By combining various important factors, a nomogram can estimate the feasibility of each patient event, such as the likelihood of death or recurrence. Thus, the nomogram has developed into an important tool for predicting clinical outcomes in various types of cancer and can provide physicians with optimal treatment options.
Aims
Our goal was to develop a reliable nomogram to predict overall survival (OS) and progression free survival (PFS) in patients with PMBCL.
Methods
Based on data from Sun Yat-Sen University Cancer Center and the First Hospital of Guangzhou Medical University,116 patients diagnosed with PMBCL were enrolled in this study. Independent prognostic factors were screened by Cox regression analysis. R-coding was used to construct nomograms predicting OS and PFS. Discriminations and corrections of the new model were evaluated using the consistency index (C-index), subject operating characteristic curves (ROC) and calibration curves, and compared with the conventional International Prognostic Index (IPI) using decision curve analysis (DCA) to assess its accuracy and benefit.
Results
Multivariate models showed that post-treatment Deauville score, Ann Arbor staging and hemoglobin level were significantly associated with PFS, while post-treatment Deauville score, MUM1 expression and Ki67 index were significantly associated with OS, and the corresponding nomograms were plotted. In the training cohort, the C-index of the nomogram for PFS and OS was 0.833 and 0.931, respectively. The C-index of the validation cohort was 0.649 and 0.661, respectively. The calibration curves of the nomogram also showed high predictive accuracy. Compared to the IPI scores,the C-index and ROC curves of the Nomogram had better results and also showed better results in the decision curve analysis, yielding better net benefits.
Conclusion
In summary, we have successfully established a valid nomogram for predicting OS and PFS in PMBCL patients, which can help clinicians to select appropriate individualized treatment for their patients.
Keyword(s): Lymphoma, Survival prediction


