
Contributions
Abstract: EP558
Type: E-Poster Presentation
Session title: Aggressive Non-Hodgkin lymphoma - Clinical
Background
: Loss of heterozygosity (LOH) in STR loci, elevated microsatellite alteration at selected tetranucleotides (EMAST) and instability of mononucleotide tandem repeats (MSI - microsatellite instability) are intrinsic features of diverse tumor cells and appropriate analysis might be used as indication for the therapy with immune checkpoint inhibitors. For primary mediastinal B-cell lymphoma (PMBCL) these molecular factors to determine the prognosis of the disease have not been described yet. A set of five mononucleotide microsatellite repeat markers BAT-25, BAT-26, NR-21, NR-24, and NR-27 might not be informative in aggressive lymphoma cases since low occurrence (up to 5%). Furthermore, in about half of the cases, the altered allele may also present in the control material, possibly characterizing not the tumor, but the genetic features of the patient. According to the literature data, EMAST-H (high degree) is associated with MSI-H in solid tumors. Overlapping combinations of enzymes of the DNA repair complex are responsible for the repair of unpaired bases and the removal of oligonucleotide insertion loops. Therefore certain defects in the DNA repair complex (MMR) may lead to both MSI and EMAST.
Aims
To analyze the frequency of LOH and EMAST in tumor cells of PMBCL patients at diagnosis and to check possible association with PD-L1 mRNA overexpression.
Methods
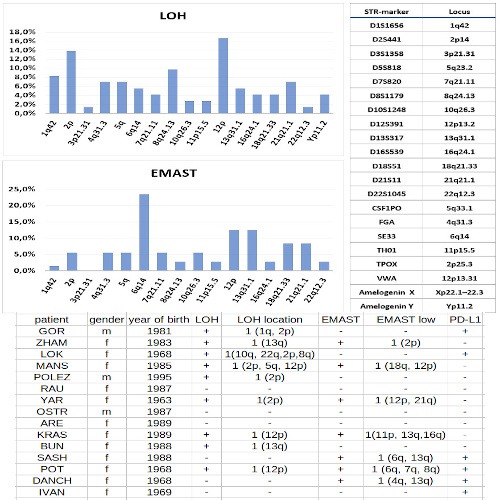
STR profiles of the DNA of tumor cells were analyzed on a cohort of 72 de novo diagnosed PMBCL patients undergoing treatment at the National Research Center for Hematology (Moscow, Russia). DNA was isolated from tumor biopsy samples taken at diagnosis. Control DNA samples were taken from the blood of patients in complete remission or from the buccal epithelium. STR-profiles for LOH and EMAST analysis were assessed by PCR with COrDIS Plus multiplex kit for amplification of 19 STR-markers and amelogenin loci (Gordiz Ltd, Russia). The fragment analysis was performed on ABI3130 Genetic Analyzer. For 15 patients LOH and EMAST status was evaluated relatively PD-L1 mRNA expression level checked at diagnosis.
Results
LOH was revealed in 37 out of 72 patients (51.4%). EMAST was found in 40 patients (55.5%); in 24 of them, EMAST was accompanied by LOH. For all EMAST-positive patients, the number of involved loci was no more than 4 from 19 (EMAST low, less than a third of the microsatellite markers panel). Among 15 patients with a known level of PD-L1 mRNA expression, six patients have no EMAST and no PD-L1 overexpression. Three patients have EMAST with 2-3 involved loci and PD-L1 overexpression. For 4 patients combination of EMAST and normal PD-L1 expression and for 2 patients no EMAST and PD-L1 overexpression were found. Standard therapy failure should be noted for patients with EMAST and PD-L1 overexpression.
Conclusion
The high incidence of LOH and EMAST in PMBCL can cause standard therapy failure in a significant number of patients. EMAST as a variant of microsatellite instability might be useful for further consideration as a predictor of response to checkpoint inhibitor therapy. The patients with EMAST and a high level of PD-L1 expression should be considered as the first candidates for immunotherapy. This study was supported by Rakfond grant 2/2020
Keyword(s): LOH, Lymphoma, Overexpression, STR-PCR
Abstract: EP558
Type: E-Poster Presentation
Session title: Aggressive Non-Hodgkin lymphoma - Clinical
Background
: Loss of heterozygosity (LOH) in STR loci, elevated microsatellite alteration at selected tetranucleotides (EMAST) and instability of mononucleotide tandem repeats (MSI - microsatellite instability) are intrinsic features of diverse tumor cells and appropriate analysis might be used as indication for the therapy with immune checkpoint inhibitors. For primary mediastinal B-cell lymphoma (PMBCL) these molecular factors to determine the prognosis of the disease have not been described yet. A set of five mononucleotide microsatellite repeat markers BAT-25, BAT-26, NR-21, NR-24, and NR-27 might not be informative in aggressive lymphoma cases since low occurrence (up to 5%). Furthermore, in about half of the cases, the altered allele may also present in the control material, possibly characterizing not the tumor, but the genetic features of the patient. According to the literature data, EMAST-H (high degree) is associated with MSI-H in solid tumors. Overlapping combinations of enzymes of the DNA repair complex are responsible for the repair of unpaired bases and the removal of oligonucleotide insertion loops. Therefore certain defects in the DNA repair complex (MMR) may lead to both MSI and EMAST.
Aims
To analyze the frequency of LOH and EMAST in tumor cells of PMBCL patients at diagnosis and to check possible association with PD-L1 mRNA overexpression.
Methods
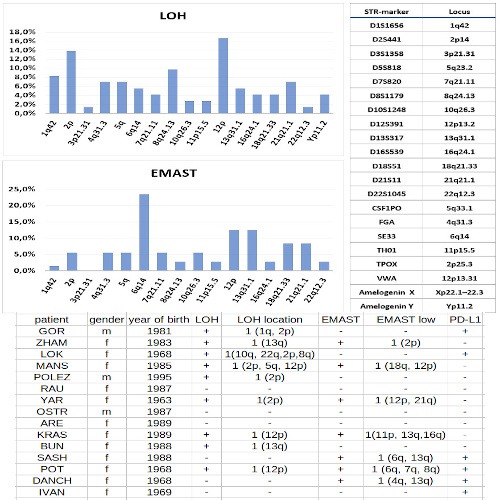
STR profiles of the DNA of tumor cells were analyzed on a cohort of 72 de novo diagnosed PMBCL patients undergoing treatment at the National Research Center for Hematology (Moscow, Russia). DNA was isolated from tumor biopsy samples taken at diagnosis. Control DNA samples were taken from the blood of patients in complete remission or from the buccal epithelium. STR-profiles for LOH and EMAST analysis were assessed by PCR with COrDIS Plus multiplex kit for amplification of 19 STR-markers and amelogenin loci (Gordiz Ltd, Russia). The fragment analysis was performed on ABI3130 Genetic Analyzer. For 15 patients LOH and EMAST status was evaluated relatively PD-L1 mRNA expression level checked at diagnosis.
Results
LOH was revealed in 37 out of 72 patients (51.4%). EMAST was found in 40 patients (55.5%); in 24 of them, EMAST was accompanied by LOH. For all EMAST-positive patients, the number of involved loci was no more than 4 from 19 (EMAST low, less than a third of the microsatellite markers panel). Among 15 patients with a known level of PD-L1 mRNA expression, six patients have no EMAST and no PD-L1 overexpression. Three patients have EMAST with 2-3 involved loci and PD-L1 overexpression. For 4 patients combination of EMAST and normal PD-L1 expression and for 2 patients no EMAST and PD-L1 overexpression were found. Standard therapy failure should be noted for patients with EMAST and PD-L1 overexpression.
Conclusion
The high incidence of LOH and EMAST in PMBCL can cause standard therapy failure in a significant number of patients. EMAST as a variant of microsatellite instability might be useful for further consideration as a predictor of response to checkpoint inhibitor therapy. The patients with EMAST and a high level of PD-L1 expression should be considered as the first candidates for immunotherapy. This study was supported by Rakfond grant 2/2020
Keyword(s): LOH, Lymphoma, Overexpression, STR-PCR


