
Contributions
Abstract: EP557
Type: E-Poster Presentation
Session title: Aggressive Non-Hodgkin lymphoma - Clinical
Background
Primary mediastinal large B-cell lymphoma (PMBCL) is distinct clinical, pathological and molecular entity of diffuse large B-cell lymphoma (DLBCL) which accounts less than 3% of all non-Hodgkin's lymphomas (NHL). The standard 1st line treatment of PMBCL does not currently exist. A lack of prospective data comparing the efficiency of R-CHOP and DA-EPOCH-R regimen, does not allow to establish the best front line treatment options. Due to the age specificity and mediastinum localisation the implementation of the International Prognostic Index (IPI) in PMBCL is limited. Thus, this clinical entity needs better definition of prognostic factors and a standard of treatment approach.
Aims
The purpose of the study was to assess the treatment outcomes (5-year OS and PFS), and the potential prognostic factors for patients with PMBCL.
Methods
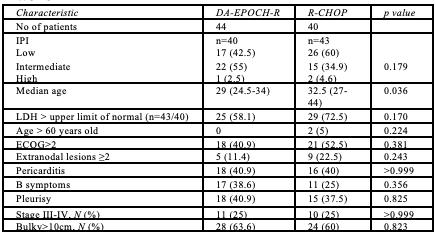
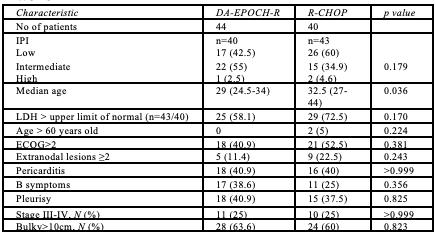
The study included 84 patients with PMBCL from 6 Ukrainian centers (Aug 2011 to Dec 2015). Patients were randomized into two groups: DA-EPOCH-R (44 pts) and R-CHOP (40 pts). Median age in DA-EPOCH-R group was 29 years (range 24.5-34) and in R-CHOP group - 32.5 (27-44) (p=0.036). Initial data included age, sex, stage, presence of B symptoms, bulky disease, ECOG, IPI score, pleuritis and pericarditis (Table 1). To analyse prognostic factors which may have impact on OS and PFS (treatment regimen, age > 40 years old, stage III-IV, ECOG≥2, > 2 exstranodal sites, elevated LDH, male sex, presence of B-symptoms, pleuritis, pericarditis, bulky disease, and number of risk factors) we provided a multivariate Cox analysis.
Results
ORR and CR rates were significantly higher in the DA-EPOCH-R group: 97.7% vs 85% (p = 0.049) and 81.8% vs 50% (p = 0.003), respectively. The 5-year PFS in the DA-EPOCH-R group reached 90.9% vs 64.1% in the R-CHOP-regimen group (p = 0.002). The 5-year OS rate was also higher in the DA-EPOCH-R arm compared to R-CHOP – 97.7% vs 73.8%, respectively (p = 0.002). The median OS was not reached in either group. Using the Cox proportional-hazards model to assess the effect of a treatment regimen on OS, a significant reduction in the risk of death was seen for the patients in the DA-EPOCH-R group [p=0.016 (HR = 0.08, 95%CI 0.01 - 0.63)]. When adjusted for age and IPI, the risk of death from PMBCL in the DA-EPOCH-R group was also lower [p=0.010 (HR=0.046, 95%CI 0.005 - 0.478)]. Moreover, the higher risk of deaths due to PMBCL occurred with an increase in number of risk factors [p=0.01 (HR = 1.8, 95%CI 1,2 – 3,0). Additionally was defined that the risk of disease progression in the first 14 months after end of treatment was associated with 3 prognostic factors: treatment regimen, > 2 extranodal sites and number of risk factors [Se 100% (95CI 80.5% - 100%); Sp 76.7% (95CI 64.0% - 86.6%)].
Conclusion
The DA-EPOCH-R regimen might overcome the effect of adverse prognostic factors. Our model could stratify patients with PMLBC and help guide selection of treatment. Thus, more prognostic studies that take into account novel biomarkers and novel prognostic features are warranted.
Keyword(s):
Abstract: EP557
Type: E-Poster Presentation
Session title: Aggressive Non-Hodgkin lymphoma - Clinical
Background
Primary mediastinal large B-cell lymphoma (PMBCL) is distinct clinical, pathological and molecular entity of diffuse large B-cell lymphoma (DLBCL) which accounts less than 3% of all non-Hodgkin's lymphomas (NHL). The standard 1st line treatment of PMBCL does not currently exist. A lack of prospective data comparing the efficiency of R-CHOP and DA-EPOCH-R regimen, does not allow to establish the best front line treatment options. Due to the age specificity and mediastinum localisation the implementation of the International Prognostic Index (IPI) in PMBCL is limited. Thus, this clinical entity needs better definition of prognostic factors and a standard of treatment approach.
Aims
The purpose of the study was to assess the treatment outcomes (5-year OS and PFS), and the potential prognostic factors for patients with PMBCL.
Methods
The study included 84 patients with PMBCL from 6 Ukrainian centers (Aug 2011 to Dec 2015). Patients were randomized into two groups: DA-EPOCH-R (44 pts) and R-CHOP (40 pts). Median age in DA-EPOCH-R group was 29 years (range 24.5-34) and in R-CHOP group - 32.5 (27-44) (p=0.036). Initial data included age, sex, stage, presence of B symptoms, bulky disease, ECOG, IPI score, pleuritis and pericarditis (Table 1). To analyse prognostic factors which may have impact on OS and PFS (treatment regimen, age > 40 years old, stage III-IV, ECOG≥2, > 2 exstranodal sites, elevated LDH, male sex, presence of B-symptoms, pleuritis, pericarditis, bulky disease, and number of risk factors) we provided a multivariate Cox analysis.
Results
ORR and CR rates were significantly higher in the DA-EPOCH-R group: 97.7% vs 85% (p = 0.049) and 81.8% vs 50% (p = 0.003), respectively. The 5-year PFS in the DA-EPOCH-R group reached 90.9% vs 64.1% in the R-CHOP-regimen group (p = 0.002). The 5-year OS rate was also higher in the DA-EPOCH-R arm compared to R-CHOP – 97.7% vs 73.8%, respectively (p = 0.002). The median OS was not reached in either group. Using the Cox proportional-hazards model to assess the effect of a treatment regimen on OS, a significant reduction in the risk of death was seen for the patients in the DA-EPOCH-R group [p=0.016 (HR = 0.08, 95%CI 0.01 - 0.63)]. When adjusted for age and IPI, the risk of death from PMBCL in the DA-EPOCH-R group was also lower [p=0.010 (HR=0.046, 95%CI 0.005 - 0.478)]. Moreover, the higher risk of deaths due to PMBCL occurred with an increase in number of risk factors [p=0.01 (HR = 1.8, 95%CI 1,2 – 3,0). Additionally was defined that the risk of disease progression in the first 14 months after end of treatment was associated with 3 prognostic factors: treatment regimen, > 2 extranodal sites and number of risk factors [Se 100% (95CI 80.5% - 100%); Sp 76.7% (95CI 64.0% - 86.6%)].
Conclusion
The DA-EPOCH-R regimen might overcome the effect of adverse prognostic factors. Our model could stratify patients with PMLBC and help guide selection of treatment. Thus, more prognostic studies that take into account novel biomarkers and novel prognostic features are warranted.
Keyword(s):


