
Contributions
Abstract: EP545
Type: E-Poster Presentation
Session title: Aggressive Non-Hodgkin lymphoma - Clinical
Background
Not all elderly pts with DLBCL will receive first-line (1L) rituximab (R)-CHOP or R-miniCHOP regimens; those who do not may have suboptimal outcomes (Williams et al. Cancer 2015). There is a lack of data regarding comorbidities or other factors (e.g. pt preference) that influence 1L treatment choice.
Aims
To use RWD to describe factors influencing 1L treatment decisions in elderly pts with DLBCL.
Methods
This study used the nationwide Flatiron Health (FH) electronic health record-derived de-identified database. The FH database is longitudinal, comprising de-identified patient-level structured and unstructured data, curated via technology-enabled abstraction. To analyze treatment rationale and pt comorbidities at diagnosis, trained clinical abstractors performed a detailed review of clinic notes. Pts aged ≥71 years at diagnosis, with a DLBCL diagnosis on or after January 1, 2011 and with follow-up until May 31, 2020, were included. Selected pts were untreated, or treated with: R-CHOP (standard dose), reduced-dose R-CHOP (<80% standard dose cyclophosphamide and doxorubicin), R-monotherapy (R-mono), R-Benda, R-CVP or R-Len. We analyzed pt demographics, comorbidities, treatment details and treatment rationale (categorized as: age, comorbidity, disease burden, International Prognostic Index [IPI], pt request, performance status [PS], or other).
Results
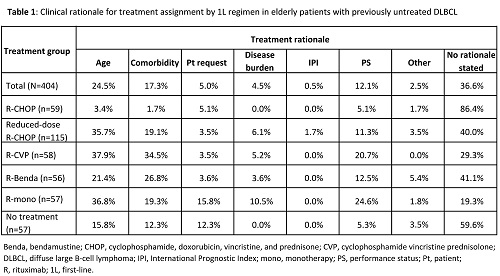
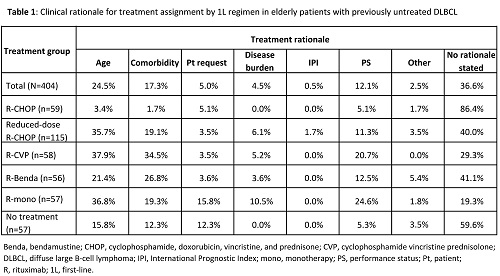
Pts (N=404) were aged ≥71 years, 94% were treated in a community setting, 90% had DLBCL-not otherwise specified, and 45% had Stage III/IV disease at diagnosis. A proportion of pts had comorbidities at diagnosis (anemia: 24.8%; arrhythmia: 19.6%; congestive heart failure: 6.7%; diabetes: 18.3%; hyperlipidemia: 36.6%; hypothyroidism: 14.6%; previous myocardial infarction: 9.7%; chronic kidney disease: 13.4%; previous stroke: 6.9%). Treatments over the study period (n [%]) were: R-Benda (56 [14]); R-CHOP (59 [15]); R-CVP (58 [14]); R-mono (57 [14]); reduced-dose R-CHOP (115 [28]); no treatment (57 [14]). R-Len-treated pts (n=2) were not included due to small sample size available. Median time from diagnosis to 1L treatment was 24 days (interquartile range: 12–39). Overall, 315 treatment rationales were given, with 122 pts having one rationale and 90 pts having ≥2 rationales. Rationale by 1L treatment is shown in the Table. Comorbidity was the principal rationale for several pts receiving: reduced-dose R-CHOP (19.1%), R-Benda (26.8%), and R-CVP (34.5%). Age was a reason for attenuated regimen selection in pts receiving: reduced-dose R-CHOP (35.7%); R-mono (36.8%); R-CVP (37.9%). No evidence of a rationale could be found for 86.4% of pts who received the standard-of-care, R-CHOP, potentially indicating that factors related to age or frailty were not significant in the choice of their treatment. In pts not receiving any treatment (systemic therapy or radiotherapy) for whom a rationale was given, this was pt request for 30.4%, and was age, comorbidities, PS, or disease burden for most other pts (>60%).
Conclusion
Age, comorbidities and PS are decisive factors in 1L treatment selection for older pts with DLBCL; disease burden or IPI are rarely stated as the rationale. The main reasons for not treating pts appear physician-driven rather than pt-requested, suggesting more pts may receive treatment if physicians have better options. If more tolerable chemotherapy-free options were available, fewer pts may refuse therapy, as illustrated by more R-mono-treated pts requesting their therapy compared with chemotherapy-treated pts. Further analysis of the impact of pt-related factors on treatment decision-making is warranted.
Keyword(s): Comorbidities, DLBCL, Elderly, Treatment
Abstract: EP545
Type: E-Poster Presentation
Session title: Aggressive Non-Hodgkin lymphoma - Clinical
Background
Not all elderly pts with DLBCL will receive first-line (1L) rituximab (R)-CHOP or R-miniCHOP regimens; those who do not may have suboptimal outcomes (Williams et al. Cancer 2015). There is a lack of data regarding comorbidities or other factors (e.g. pt preference) that influence 1L treatment choice.
Aims
To use RWD to describe factors influencing 1L treatment decisions in elderly pts with DLBCL.
Methods
This study used the nationwide Flatiron Health (FH) electronic health record-derived de-identified database. The FH database is longitudinal, comprising de-identified patient-level structured and unstructured data, curated via technology-enabled abstraction. To analyze treatment rationale and pt comorbidities at diagnosis, trained clinical abstractors performed a detailed review of clinic notes. Pts aged ≥71 years at diagnosis, with a DLBCL diagnosis on or after January 1, 2011 and with follow-up until May 31, 2020, were included. Selected pts were untreated, or treated with: R-CHOP (standard dose), reduced-dose R-CHOP (<80% standard dose cyclophosphamide and doxorubicin), R-monotherapy (R-mono), R-Benda, R-CVP or R-Len. We analyzed pt demographics, comorbidities, treatment details and treatment rationale (categorized as: age, comorbidity, disease burden, International Prognostic Index [IPI], pt request, performance status [PS], or other).
Results
Pts (N=404) were aged ≥71 years, 94% were treated in a community setting, 90% had DLBCL-not otherwise specified, and 45% had Stage III/IV disease at diagnosis. A proportion of pts had comorbidities at diagnosis (anemia: 24.8%; arrhythmia: 19.6%; congestive heart failure: 6.7%; diabetes: 18.3%; hyperlipidemia: 36.6%; hypothyroidism: 14.6%; previous myocardial infarction: 9.7%; chronic kidney disease: 13.4%; previous stroke: 6.9%). Treatments over the study period (n [%]) were: R-Benda (56 [14]); R-CHOP (59 [15]); R-CVP (58 [14]); R-mono (57 [14]); reduced-dose R-CHOP (115 [28]); no treatment (57 [14]). R-Len-treated pts (n=2) were not included due to small sample size available. Median time from diagnosis to 1L treatment was 24 days (interquartile range: 12–39). Overall, 315 treatment rationales were given, with 122 pts having one rationale and 90 pts having ≥2 rationales. Rationale by 1L treatment is shown in the Table. Comorbidity was the principal rationale for several pts receiving: reduced-dose R-CHOP (19.1%), R-Benda (26.8%), and R-CVP (34.5%). Age was a reason for attenuated regimen selection in pts receiving: reduced-dose R-CHOP (35.7%); R-mono (36.8%); R-CVP (37.9%). No evidence of a rationale could be found for 86.4% of pts who received the standard-of-care, R-CHOP, potentially indicating that factors related to age or frailty were not significant in the choice of their treatment. In pts not receiving any treatment (systemic therapy or radiotherapy) for whom a rationale was given, this was pt request for 30.4%, and was age, comorbidities, PS, or disease burden for most other pts (>60%).
Conclusion
Age, comorbidities and PS are decisive factors in 1L treatment selection for older pts with DLBCL; disease burden or IPI are rarely stated as the rationale. The main reasons for not treating pts appear physician-driven rather than pt-requested, suggesting more pts may receive treatment if physicians have better options. If more tolerable chemotherapy-free options were available, fewer pts may refuse therapy, as illustrated by more R-mono-treated pts requesting their therapy compared with chemotherapy-treated pts. Further analysis of the impact of pt-related factors on treatment decision-making is warranted.
Keyword(s): Comorbidities, DLBCL, Elderly, Treatment


