
Contributions
Abstract: EP538
Type: E-Poster Presentation
Session title: Aggressive Non-Hodgkin lymphoma - Clinical
Background
Pediatric T-cell lymphoblastic lymphoma (T-LBL) arises from the malignant transformation of immature T-cells. T-LBL is characterized by massive infiltration of blasts in the mediastinum and lymph nodes mostly without or occasionally with low percentages of blasts in the bone marrow (<25%). Patients are assigned to different treatment regimens based on Murphy staging, which is determined by disease localization and dissemination. These treatment protocols have not been essentially changed over the last decades, showing the need to improve our knowledge on T-LBL.
Aims
This study investigated the clinical characteristics and the occurrence of secondary malignancies and comorbidities in an unselected cohort of pediatric T-LBL patients.
Methods
We present a retrospective pediatric T-LBL cohort (n=88) for patients who were diagnosed between January 2007 and September 2020 and who were treated according to the EURO-LB02 protocol in one of the former pediatric oncology centers in the Netherlands.
Results
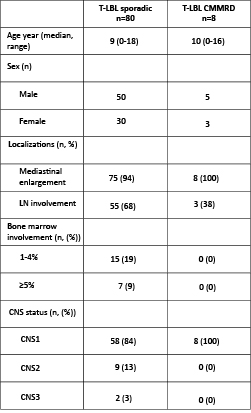
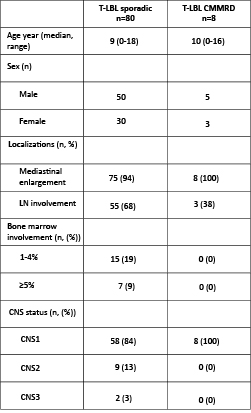
Median age at diagnosis for this T-LBL cohort was 9 years (range 0-18), with a male to female ratio of 1.7:1. Disease localizations mainly involved the mediastinum which was enlarged in 94% of the patients and enlarged lymph nodes in 68% of the patients. Nine percent of the patients had evidence of blast infiltration in the bone marrow (BM) (range 5-16% blasts). Two patients presented with CNS3 and had more than 5 white blood cells/µl (WBC) in the cerebral spinal fluid (CSF), whereas nine patients presented with CNS2 and having less than 5 WBC/µl CSF fluid. In total 10.2% (9/88) of the patients were diagnosed with a cancer predisposition syndrome, almost exclusively constitutional mismatch repair deficiency (CMMRD) (8/88), based on their presentation with multiple café-au-lait maculae in all patients and a history of previous or secondary cancers in various patients. All CMMRD patients in our cohort had biallelic germline mutations in either PMS2 or MSH6. Clinical and patient characteristics of CMMRD patients at time of T-LBL diagnosis were compared to sporadic T-LBL patients and summarized in Table 1. Whereas their clinical presentation was comparable, the percentage of CMMRD patients who had one or multiple enlarged lymph nodes seemed lower than for sporadic patients albeit not significant (p=0.1179). None of the CMMRD patients presented with BM involvement at T-LBL diagnosis in comparison to 25% of sporadic T-LBL patients who had >1% blasts in their BM at time of diagnosis (and 8% having >5% blasts). Two sporadic patients presented with CNS3 while nine patients had CNS2 (9/80) in contrast to none of the CMMRD patients, indicating that the T-LBL manifestation for CMMRD patients is more localized compared to sporadic T-LBL patients. Currently, the presence of preceding or secondary (childhood) malignancies is the main indicator for the presence of an underlying cancer predisposition syndrome. Therefore, diagnosis of a cancer predisposition syndrome is often missed at time of diagnosis of the first (childhood) malignancy, highlighting the alertness of the treating physician as crucial factor for diagnosis.
Conclusion
This study describes the high prevalence of CMMRD patients in a complete T-LBL cohort. As the frequency of an underlying predisposition syndrome among T-LBL patients may be underestimated at present, we advocate for screening all pediatric T-LBL patients with café-au-lait maculae for the presence of germline mutations in mismatch repair genes.
Keyword(s): T cell lymphoma
Abstract: EP538
Type: E-Poster Presentation
Session title: Aggressive Non-Hodgkin lymphoma - Clinical
Background
Pediatric T-cell lymphoblastic lymphoma (T-LBL) arises from the malignant transformation of immature T-cells. T-LBL is characterized by massive infiltration of blasts in the mediastinum and lymph nodes mostly without or occasionally with low percentages of blasts in the bone marrow (<25%). Patients are assigned to different treatment regimens based on Murphy staging, which is determined by disease localization and dissemination. These treatment protocols have not been essentially changed over the last decades, showing the need to improve our knowledge on T-LBL.
Aims
This study investigated the clinical characteristics and the occurrence of secondary malignancies and comorbidities in an unselected cohort of pediatric T-LBL patients.
Methods
We present a retrospective pediatric T-LBL cohort (n=88) for patients who were diagnosed between January 2007 and September 2020 and who were treated according to the EURO-LB02 protocol in one of the former pediatric oncology centers in the Netherlands.
Results
Median age at diagnosis for this T-LBL cohort was 9 years (range 0-18), with a male to female ratio of 1.7:1. Disease localizations mainly involved the mediastinum which was enlarged in 94% of the patients and enlarged lymph nodes in 68% of the patients. Nine percent of the patients had evidence of blast infiltration in the bone marrow (BM) (range 5-16% blasts). Two patients presented with CNS3 and had more than 5 white blood cells/µl (WBC) in the cerebral spinal fluid (CSF), whereas nine patients presented with CNS2 and having less than 5 WBC/µl CSF fluid. In total 10.2% (9/88) of the patients were diagnosed with a cancer predisposition syndrome, almost exclusively constitutional mismatch repair deficiency (CMMRD) (8/88), based on their presentation with multiple café-au-lait maculae in all patients and a history of previous or secondary cancers in various patients. All CMMRD patients in our cohort had biallelic germline mutations in either PMS2 or MSH6. Clinical and patient characteristics of CMMRD patients at time of T-LBL diagnosis were compared to sporadic T-LBL patients and summarized in Table 1. Whereas their clinical presentation was comparable, the percentage of CMMRD patients who had one or multiple enlarged lymph nodes seemed lower than for sporadic patients albeit not significant (p=0.1179). None of the CMMRD patients presented with BM involvement at T-LBL diagnosis in comparison to 25% of sporadic T-LBL patients who had >1% blasts in their BM at time of diagnosis (and 8% having >5% blasts). Two sporadic patients presented with CNS3 while nine patients had CNS2 (9/80) in contrast to none of the CMMRD patients, indicating that the T-LBL manifestation for CMMRD patients is more localized compared to sporadic T-LBL patients. Currently, the presence of preceding or secondary (childhood) malignancies is the main indicator for the presence of an underlying cancer predisposition syndrome. Therefore, diagnosis of a cancer predisposition syndrome is often missed at time of diagnosis of the first (childhood) malignancy, highlighting the alertness of the treating physician as crucial factor for diagnosis.
Conclusion
This study describes the high prevalence of CMMRD patients in a complete T-LBL cohort. As the frequency of an underlying predisposition syndrome among T-LBL patients may be underestimated at present, we advocate for screening all pediatric T-LBL patients with café-au-lait maculae for the presence of germline mutations in mismatch repair genes.
Keyword(s): T cell lymphoma


