
Contributions
Abstract: EP523
Type: E-Poster Presentation
Session title: Aggressive Non-Hodgkin lymphoma - Clinical
Background
Diffuse Large B Cell Lymphoma (DLBCL) is the most common type of non-Hodgkin Lymphoma (NHL) and accounts for about 40% of all NHL[1]. There are several treatment options used in the management of DLBCL in older patients (>80 years old) including curative anthracycline-based regimens and palliative regimens; however, this age group appears to be under-represented in clinical trials likely due to concerns regarding patient comorbidities and treatment tolerance. R-MiniCHOP has been shown to be safe and effective in >80 year olds[2]. We present novel data from a multi-centre UK study with a focus on survival outlooks for DLBCL in the >80 age group.
Aims
To assess wether there is any significant difference in overall survival between intensive/reduced intensity/palliative chemotherapy/palliative without chemotherapy, in the frail over 80 age DLBCL group. With an aim to try and inform future treatment decisions.
Methods
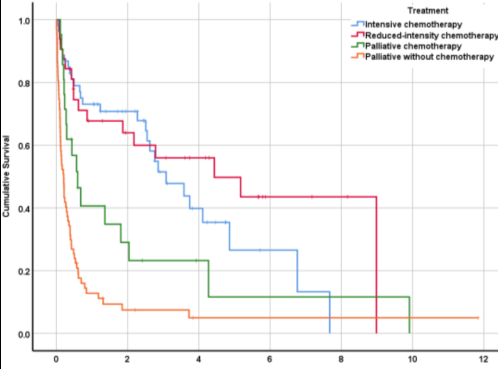
Patient demographics and survival data were retrospectively collected (N=173) from Norwich and Sheffield University Hospitals. Four treatment groups were included for analyses: intensive chemotherapy (full dose RCHOP/RGCVP/R-PMitCEBO, N=53); reduced-intensity chemotherapy (R-miniCHOP/RCVP, N=32); palliative chemotherapy (VEDEX/Chlorambucil/Etoposide, N=21) and palliative without chemotherapy (steroids/palliative radiotherapy, N=67). Overall survival (OS) by age (Spearman’s correlation) and sex (Mann-Whitney U) was analysed. Median survival by treatment was calculated and a Kaplan-Meier plot was generated. We performed a multivariate analysis (Cox regression) which assessed both age and treatment in relation to OS. Post-hoc Kruskal-Wallis testing detailed specific differences between treatment groups.
Results
Age was significantly negatively correlated with OS (p=.011) whereas there was no significant difference in OS between sexes (p=.653). The overall median OS was 0.57 years. Median OS values by treatment were 1.95 years (intensive), 2.06 years (reduced-intensity), 0.57 years (palliative) and 0.21 years (palliative without chemotherapy). The subsequent multivariate survival analysis showed OS varied significantly between treatment groups (p<.001); in this model, age did not retain its significance (p=0.824). Post-hoc testing revealed treatment differences were primarily driven by palliative (without chemotherapy) conferring a significantly lower OS versus all other treatments. Figure 1 shows how OS varies by treatment group. Of note, reduced-intensity chemotherapy resulted in a higher median OS than intensive chemotherapy (2.06 years vs 1.95 years), however this finding was not significantly different and larger studies may be useful in detecting an effect.
Conclusion
To conclude, we have shown that age and treatment each significantly predict OS, but when these variables are included together in a multivariate analysis, treatment remains the only significant predictor, possibly due to patients being pre-selected into treatment groups by age. Although not significantly greater than the intensive treatment OS, the reduced-intensity OS was the largest of all treatments included. This may be due to the elderly population having difficulty tolerating intensive chemotherapy leading to treatment ‘holidays’, an overall decline in health and a lower OS than reduced-intensity chemotherapy - it is therefore highlighted here as a potential point of future research. Better powered analyses should further examine patient factors such as treatment tolerability, complication rates and late effects which may impact on OS in this frail study population.
Keyword(s): Chemotherapy, Diffuse large B cell lymphoma, Old, Survival
Abstract: EP523
Type: E-Poster Presentation
Session title: Aggressive Non-Hodgkin lymphoma - Clinical
Background
Diffuse Large B Cell Lymphoma (DLBCL) is the most common type of non-Hodgkin Lymphoma (NHL) and accounts for about 40% of all NHL[1]. There are several treatment options used in the management of DLBCL in older patients (>80 years old) including curative anthracycline-based regimens and palliative regimens; however, this age group appears to be under-represented in clinical trials likely due to concerns regarding patient comorbidities and treatment tolerance. R-MiniCHOP has been shown to be safe and effective in >80 year olds[2]. We present novel data from a multi-centre UK study with a focus on survival outlooks for DLBCL in the >80 age group.
Aims
To assess wether there is any significant difference in overall survival between intensive/reduced intensity/palliative chemotherapy/palliative without chemotherapy, in the frail over 80 age DLBCL group. With an aim to try and inform future treatment decisions.
Methods
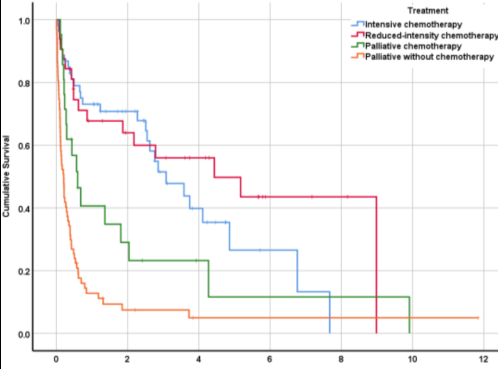
Patient demographics and survival data were retrospectively collected (N=173) from Norwich and Sheffield University Hospitals. Four treatment groups were included for analyses: intensive chemotherapy (full dose RCHOP/RGCVP/R-PMitCEBO, N=53); reduced-intensity chemotherapy (R-miniCHOP/RCVP, N=32); palliative chemotherapy (VEDEX/Chlorambucil/Etoposide, N=21) and palliative without chemotherapy (steroids/palliative radiotherapy, N=67). Overall survival (OS) by age (Spearman’s correlation) and sex (Mann-Whitney U) was analysed. Median survival by treatment was calculated and a Kaplan-Meier plot was generated. We performed a multivariate analysis (Cox regression) which assessed both age and treatment in relation to OS. Post-hoc Kruskal-Wallis testing detailed specific differences between treatment groups.
Results
Age was significantly negatively correlated with OS (p=.011) whereas there was no significant difference in OS between sexes (p=.653). The overall median OS was 0.57 years. Median OS values by treatment were 1.95 years (intensive), 2.06 years (reduced-intensity), 0.57 years (palliative) and 0.21 years (palliative without chemotherapy). The subsequent multivariate survival analysis showed OS varied significantly between treatment groups (p<.001); in this model, age did not retain its significance (p=0.824). Post-hoc testing revealed treatment differences were primarily driven by palliative (without chemotherapy) conferring a significantly lower OS versus all other treatments. Figure 1 shows how OS varies by treatment group. Of note, reduced-intensity chemotherapy resulted in a higher median OS than intensive chemotherapy (2.06 years vs 1.95 years), however this finding was not significantly different and larger studies may be useful in detecting an effect.
Conclusion
To conclude, we have shown that age and treatment each significantly predict OS, but when these variables are included together in a multivariate analysis, treatment remains the only significant predictor, possibly due to patients being pre-selected into treatment groups by age. Although not significantly greater than the intensive treatment OS, the reduced-intensity OS was the largest of all treatments included. This may be due to the elderly population having difficulty tolerating intensive chemotherapy leading to treatment ‘holidays’, an overall decline in health and a lower OS than reduced-intensity chemotherapy - it is therefore highlighted here as a potential point of future research. Better powered analyses should further examine patient factors such as treatment tolerability, complication rates and late effects which may impact on OS in this frail study population.
Keyword(s): Chemotherapy, Diffuse large B cell lymphoma, Old, Survival


