
Contributions
Abstract: EP517
Type: E-Poster Presentation
Session title: Aggressive Non-Hodgkin lymphoma - Clinical
Background
Diffuse large B-cell lymphoma (DLBCL) is the most common subtype of non-Hodgkin lymphoma with a large spread in outcome. Part of the heterogeneity can be explained by genetic abnormalities, such as MYC oncogene rearrangements. MYC rearrangements are often accompanied by BCL2 and/or BCL6 rearrangements and occur in approximately 10-15% of patients and has been associated with poor prognosis.
Aims
The aim of this study was to analyse the patterns of 18F-fluorodeoxyglucose positron emission tomography computed tomography (18F-FDG PET/CT) response in DLBCL patients with MYC rearrangements (MYC+) compared to the response patterns of DLBCL patients without MYC rearrangements (MYC-).
Methods
80 MYC+ DLBCL patients included in the HOVON-130 study, and 126 MYC- DLBCL patients in the HOVON-84 study were analysed. MYC, BCL2 and BCL6 positivity was assessed by Fluorescence In Situ Hybridization. For the MYC+ patients, 25% of patients had a single hit, and 75% a double or triple hit lymphoma. MYC+ patients were treated with 6 cycles of rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP21) combined with lenalidomide, followed by 2 gifts of rituximab. MYC- patients were randomized between 6-8 cycles of R-CHOP14 with or without rituximab intensification. 18F-FDG PET/CT scans were performed at baseline, after 3-4 cycles of treatment (I-PET) and at end of treatment (EoT-PET). All scans were centrally reviewed and evaluated according to the Deauville 5-point scale (DS). DS 1-3 was regarded as PET-negative and DS 4-5 as PET-positive. I-PET and EoT-PET positivity rates were compared between MYC+ and MYC- groups using the chi-square test for independence. Positive predictive value (PPV) and negative predictive value (NPV) of I-PET and EoT-PET were calculated for 2-year overall survival, defined as date of registration to death, as outcome. Metabolic tumour volume was calculated at baseline, I-PET and EoT-PET using the ACCURATE tool.
Results
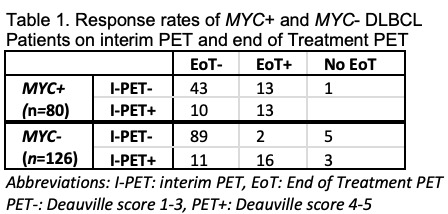
As expected, MYC+ DLBCL patients had significantly more positive EoT-PET scans compared to MYC- patients (33% (26/79) vs 15% (18/118), p=0.004, Table 1). I-PET response rates were comparable between MYC+ and MYC- DLBCL patients. Of the I-PET negative patients 23% (13/56) of the MYC+ patients turned out positive at EoT-PET, compared to 2% (2/91) for the MYC- patients. In total, 81% (21/26) of EoT-PET positive MYC+ patients presented with new nodal and/or extranodal lesions compared to I-PET, and 35% of EoT-PET positive MYC+ patients showed new lesions at EoT-PET in regions that were not initially involved at baseline. For the MYC- patients, 22% (4/18) of the EoT-positive patients presented with new nodal and/or extranodal lesions compared to I-PET, and 5.6% of the EoT-PET positive patients had new lesions in regions that were not initially involved at baseline. Out of the MYC+ patients that were positive at I-PET and EoT-PET, 60% showed enhancement of tumor volume at EoT-PET, this was the case of 38% of the MYC- DLBCL patients. 50% (13/26) of the EoT-PET positive MYC+ patients had negative I-PET assessment, compared to 11% (2/18) of the EoT-PET positive MYC- patients. Positive predictive values of I-PET and EoT-PET were higher for the MYC+ DLBCL patients compared to MYC- DLBCL patients (range: 31.6%>61.5%), whereas negative predictive values were higher for MYC- DLBCL patients (range: 81.8%>94.1%).
Conclusion
MYC+ DLBCL patients demonstrate specific response patterns, therefore I-PET is less predictive in MYC+ DLBCL patients.
Keyword(s): Diffuse large B cell lymphoma, PET, Prediction
Abstract: EP517
Type: E-Poster Presentation
Session title: Aggressive Non-Hodgkin lymphoma - Clinical
Background
Diffuse large B-cell lymphoma (DLBCL) is the most common subtype of non-Hodgkin lymphoma with a large spread in outcome. Part of the heterogeneity can be explained by genetic abnormalities, such as MYC oncogene rearrangements. MYC rearrangements are often accompanied by BCL2 and/or BCL6 rearrangements and occur in approximately 10-15% of patients and has been associated with poor prognosis.
Aims
The aim of this study was to analyse the patterns of 18F-fluorodeoxyglucose positron emission tomography computed tomography (18F-FDG PET/CT) response in DLBCL patients with MYC rearrangements (MYC+) compared to the response patterns of DLBCL patients without MYC rearrangements (MYC-).
Methods
80 MYC+ DLBCL patients included in the HOVON-130 study, and 126 MYC- DLBCL patients in the HOVON-84 study were analysed. MYC, BCL2 and BCL6 positivity was assessed by Fluorescence In Situ Hybridization. For the MYC+ patients, 25% of patients had a single hit, and 75% a double or triple hit lymphoma. MYC+ patients were treated with 6 cycles of rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP21) combined with lenalidomide, followed by 2 gifts of rituximab. MYC- patients were randomized between 6-8 cycles of R-CHOP14 with or without rituximab intensification. 18F-FDG PET/CT scans were performed at baseline, after 3-4 cycles of treatment (I-PET) and at end of treatment (EoT-PET). All scans were centrally reviewed and evaluated according to the Deauville 5-point scale (DS). DS 1-3 was regarded as PET-negative and DS 4-5 as PET-positive. I-PET and EoT-PET positivity rates were compared between MYC+ and MYC- groups using the chi-square test for independence. Positive predictive value (PPV) and negative predictive value (NPV) of I-PET and EoT-PET were calculated for 2-year overall survival, defined as date of registration to death, as outcome. Metabolic tumour volume was calculated at baseline, I-PET and EoT-PET using the ACCURATE tool.
Results
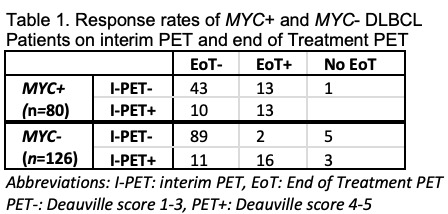
As expected, MYC+ DLBCL patients had significantly more positive EoT-PET scans compared to MYC- patients (33% (26/79) vs 15% (18/118), p=0.004, Table 1). I-PET response rates were comparable between MYC+ and MYC- DLBCL patients. Of the I-PET negative patients 23% (13/56) of the MYC+ patients turned out positive at EoT-PET, compared to 2% (2/91) for the MYC- patients. In total, 81% (21/26) of EoT-PET positive MYC+ patients presented with new nodal and/or extranodal lesions compared to I-PET, and 35% of EoT-PET positive MYC+ patients showed new lesions at EoT-PET in regions that were not initially involved at baseline. For the MYC- patients, 22% (4/18) of the EoT-positive patients presented with new nodal and/or extranodal lesions compared to I-PET, and 5.6% of the EoT-PET positive patients had new lesions in regions that were not initially involved at baseline. Out of the MYC+ patients that were positive at I-PET and EoT-PET, 60% showed enhancement of tumor volume at EoT-PET, this was the case of 38% of the MYC- DLBCL patients. 50% (13/26) of the EoT-PET positive MYC+ patients had negative I-PET assessment, compared to 11% (2/18) of the EoT-PET positive MYC- patients. Positive predictive values of I-PET and EoT-PET were higher for the MYC+ DLBCL patients compared to MYC- DLBCL patients (range: 31.6%>61.5%), whereas negative predictive values were higher for MYC- DLBCL patients (range: 81.8%>94.1%).
Conclusion
MYC+ DLBCL patients demonstrate specific response patterns, therefore I-PET is less predictive in MYC+ DLBCL patients.
Keyword(s): Diffuse large B cell lymphoma, PET, Prediction


