
Contributions
Abstract: EP515
Type: E-Poster Presentation
Session title: Aggressive Non-Hodgkin lymphoma - Clinical
Background
Post-Transplant Lymphoproliferative Disorder (PTLD) is a complication of transplantation that often arises due to reactivation of the Epstein-Barr Virus (EBV). Given the rarity of this disease, a full understanding of its presentation and optimal therapies has yet to be determined.
Aims
To describe the presentation, prognostic features, therapies, and outcomes of PTLD.
Methods
A multicenter retrospective analysis was performed utilizing data from kidney transplant patients (pts) who developed PTLD at the Hospital of the University of Pennsylvania and the Cleveland Clinic. The association between categorical variables and clinical response were assessed via Fisher’s exact testing.
Results
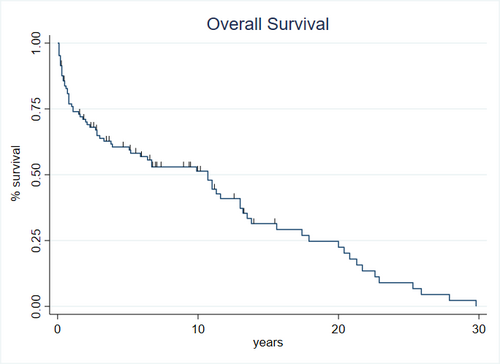
117 pts had diagnoses of PTLD after kidney transplantation. The median age at PTLD diagnosis was 52 yrs (range 17-89 yrs), and the median time from transplantation to diagnosis was 3.6 yrs (range: 7 days-36 yrs). Pt characteristics included: 84% Caucasian, 57% male, and 11% combined kidney and pancreas transplant patients. 68% pts had received unrelated donor transplants; 41% had prior rejection episodes. PTLD histology was 72% monomorphic and 28% polymorphic. Polymorphic PTLD was more likely to be EBV+ than monomorphic PTLD (81% vs. 54%, p=0.05). At diagnosis, immunosuppression included: steroids (95%), mycophenolate (44%), azathioprine (40%), sirolimus (30%), cyclosporine (46%), and/or tacrolimus (45%). Common PTLD symptoms included fever (34%), pain (38%), weight loss (30%), fatigue (30%), and/or mass (26%). The most common sites of involvement were lymph nodes (64%), kidney allograft (22%), and/or GI tract (17%). At diagnosis, 61% of patients’ tumors were EBV+ and 59% of patients had elevated serum LDH. Overall, the majority of pts responded to first-line PTLD therapy, with 61% CR and 14% PR. Reduction of immunosuppression (RI) alone (36% of pts) led to 48% CR and 12% PR; RI with rituximab (16%) led to 47% CR and 7% PR; and RI with chemotherapy (14%) resulted in 58% CR and 42% PR. Patients treated with RI as well as resection (n=18) of their limited stage disease had better outcomes (p=0.05). Overall survival for all patients was 10.7 years (95% CI: 5.1-13 years) (Figure), suggesting that a majority of patients achieve long term survival. PTLD patients <40 yrs were more likely to achieve CR after first line therapy (91% vs. 50%, p<0.001), have allograft involvement (43% vs. 14%, p=0.003), and have a polymorphic histology (52% vs. 17%, p=0.002).
Allograft involvement tended to occur sooner after transplant, occurring a median of 70 days (IQR: 29 days-2.6 yrs), whereas PTLD with no allograft involvement occurred a median of 5.4 yrs (IQR: 2.0-13.0 yrs, p=0.001). Allograft involvement was more likely to present with allograft failure (48% vs. 17%, p=0.003). PTLD with allograft involvement were more likely to achieve CR after first therapy than regular PTLD (88% vs. 54%, p=0.007) and often responded well to complete resection and RI.
Conclusion
Pts with PTLD may achieve a CR through different initial therapies. Younger patients and those able to undergo complete resection of disease and RI had better prognoses. Allograft involvement by PTLD carries a good prognosis and should be identified and treated differently from other presentations.
Keyword(s): Non-Hodgkin's lymphoma, Transplant
Abstract: EP515
Type: E-Poster Presentation
Session title: Aggressive Non-Hodgkin lymphoma - Clinical
Background
Post-Transplant Lymphoproliferative Disorder (PTLD) is a complication of transplantation that often arises due to reactivation of the Epstein-Barr Virus (EBV). Given the rarity of this disease, a full understanding of its presentation and optimal therapies has yet to be determined.
Aims
To describe the presentation, prognostic features, therapies, and outcomes of PTLD.
Methods
A multicenter retrospective analysis was performed utilizing data from kidney transplant patients (pts) who developed PTLD at the Hospital of the University of Pennsylvania and the Cleveland Clinic. The association between categorical variables and clinical response were assessed via Fisher’s exact testing.
Results
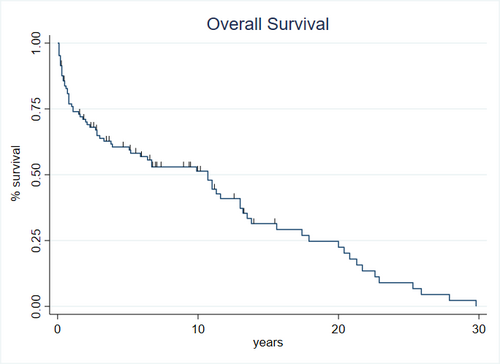
117 pts had diagnoses of PTLD after kidney transplantation. The median age at PTLD diagnosis was 52 yrs (range 17-89 yrs), and the median time from transplantation to diagnosis was 3.6 yrs (range: 7 days-36 yrs). Pt characteristics included: 84% Caucasian, 57% male, and 11% combined kidney and pancreas transplant patients. 68% pts had received unrelated donor transplants; 41% had prior rejection episodes. PTLD histology was 72% monomorphic and 28% polymorphic. Polymorphic PTLD was more likely to be EBV+ than monomorphic PTLD (81% vs. 54%, p=0.05). At diagnosis, immunosuppression included: steroids (95%), mycophenolate (44%), azathioprine (40%), sirolimus (30%), cyclosporine (46%), and/or tacrolimus (45%). Common PTLD symptoms included fever (34%), pain (38%), weight loss (30%), fatigue (30%), and/or mass (26%). The most common sites of involvement were lymph nodes (64%), kidney allograft (22%), and/or GI tract (17%). At diagnosis, 61% of patients’ tumors were EBV+ and 59% of patients had elevated serum LDH. Overall, the majority of pts responded to first-line PTLD therapy, with 61% CR and 14% PR. Reduction of immunosuppression (RI) alone (36% of pts) led to 48% CR and 12% PR; RI with rituximab (16%) led to 47% CR and 7% PR; and RI with chemotherapy (14%) resulted in 58% CR and 42% PR. Patients treated with RI as well as resection (n=18) of their limited stage disease had better outcomes (p=0.05). Overall survival for all patients was 10.7 years (95% CI: 5.1-13 years) (Figure), suggesting that a majority of patients achieve long term survival. PTLD patients <40 yrs were more likely to achieve CR after first line therapy (91% vs. 50%, p<0.001), have allograft involvement (43% vs. 14%, p=0.003), and have a polymorphic histology (52% vs. 17%, p=0.002).
Allograft involvement tended to occur sooner after transplant, occurring a median of 70 days (IQR: 29 days-2.6 yrs), whereas PTLD with no allograft involvement occurred a median of 5.4 yrs (IQR: 2.0-13.0 yrs, p=0.001). Allograft involvement was more likely to present with allograft failure (48% vs. 17%, p=0.003). PTLD with allograft involvement were more likely to achieve CR after first therapy than regular PTLD (88% vs. 54%, p=0.007) and often responded well to complete resection and RI.
Conclusion
Pts with PTLD may achieve a CR through different initial therapies. Younger patients and those able to undergo complete resection of disease and RI had better prognoses. Allograft involvement by PTLD carries a good prognosis and should be identified and treated differently from other presentations.
Keyword(s): Non-Hodgkin's lymphoma, Transplant


