
Contributions
Abstract: EP504
Type: E-Poster Presentation
Session title: Aggressive Non-Hodgkin lymphoma - Clinical
Background
Diffuse large B-cell lymphoma (DLBCL) is the most common non-Hodgkin lymphoma. In the UK, the NHS Cancer Plan in the year 2000 announced the NHS urgent cancer referral pathway - the ‘Two Week Wait’ diagnosis pathway is an initiative for the implementation of all suspected cancer patients (pts). This national pathway is designed to expedite urgent specialist referral (within 2 weeks) for pts whose signs or symptoms were suggestive of cancer, with the aspiration to enable early diagnosis and improve patient outcomes.
Aims
We wished to examine real-world practice, treatment and outcome patterns in older pts, with a focus on the effect of route to initial diagnosis to outcome. No prior published analyses have examined the effect of the diagnostic pathway on pt survival with aggressive lymphoma.
Methods
Data were extracted from Public Health England’s National Cancer Registration and Analysis Service between 2013-2015 which included route to initial diagnosis, disease characteristics, socio-economic deprivation quintiles, and survival. The Systemic Anti-Cancer Therapy dataset identified front-line regimens, cycle number and doses. Overall survival (OS) was defined from DLBCL diagnosis until time of death from any cause and differences in OS were determined by log-rank tests. Lymphoma-specific survival (LSS) was defined from DLBCL diagnosis until the time of death from DLBCL, with censoring occurring at the cause of death for causes other than DLBCL. To account for the impact of multiple variables on survival, a cox-regression model was implemented using the ‘stcox’ command. Differences in proportions for descriptive statistics were tested with a 2-sided Z-test. Data were interrogated to explore potential associations between route to diagnosis and baseline characteristics with OS and LSS.
Results
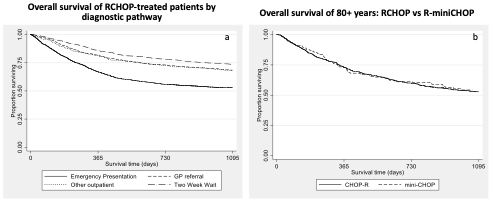
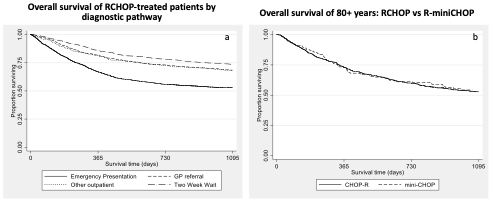
A total of 9186 DLBCL pts ≥65 years across a 3-year period (2013-2015) were identified. Median follow-up of the whole cohort was 2.1 years. 68% were aged 65-79 years. Gender distribution was equal. 4536 presented with stage III-IV (61%). Routes to initial diagnosis were emergency (34%), NHS urgent cancer referral pathway (29%) and standard GP referral (25%). The most common regimen was R-CHOP (n=4392), administered to 80.5% of those with a known regimen. 313 pts received R-miniCHOP (7% of all R-CHOP). For all pts, 3-year OS for those 65-79 years was 57% (95% confidence interval (CI) 56%>58%) and for ≥80 years was 32% (95% CI 30%>33%). 3-year OS for R-CHOP-treated pts diagnosed via emergency presentation (n=1160) was 54% (reference 1.00, GP referrals (Fig A): fully-adjusted hazard ratio (HR) 1.63 (95% CI:1.43-1.86, p<0.01) and 75% (fully-adjusted HR 0.81 (95% CI:0.71-0.93, p<0.01) on the NHS urgent cancer referral pathway (n=1635). NHS urgent cancer referral pathway retained its association with an improved LSS (HR 0.71, 95% CI 0.53-0.95, p=0.02), whilst pts with an emergency presentation had a significantly worse LSS by MVA (HR 1.95, 95% CI 1.49-2.54, p<0.01). 3-year OS was equivalent (54%) for both R-miniCHOP and R-CHOP in those ≥80 years (Fig B).
Conclusion
Our large, comprehensive real world practice analysis are the first to show that the NHS urgent cancer referral pathway leads to superior lymphoma-specific and overall survival in R-CHOP treated DLBCL pts even after adjusting for multiple confounders. Equivalent survival for R-CHOP and R-mini-CHOP in those ≥80 years supports the use of the latter in this setting.
Keyword(s):
Abstract: EP504
Type: E-Poster Presentation
Session title: Aggressive Non-Hodgkin lymphoma - Clinical
Background
Diffuse large B-cell lymphoma (DLBCL) is the most common non-Hodgkin lymphoma. In the UK, the NHS Cancer Plan in the year 2000 announced the NHS urgent cancer referral pathway - the ‘Two Week Wait’ diagnosis pathway is an initiative for the implementation of all suspected cancer patients (pts). This national pathway is designed to expedite urgent specialist referral (within 2 weeks) for pts whose signs or symptoms were suggestive of cancer, with the aspiration to enable early diagnosis and improve patient outcomes.
Aims
We wished to examine real-world practice, treatment and outcome patterns in older pts, with a focus on the effect of route to initial diagnosis to outcome. No prior published analyses have examined the effect of the diagnostic pathway on pt survival with aggressive lymphoma.
Methods
Data were extracted from Public Health England’s National Cancer Registration and Analysis Service between 2013-2015 which included route to initial diagnosis, disease characteristics, socio-economic deprivation quintiles, and survival. The Systemic Anti-Cancer Therapy dataset identified front-line regimens, cycle number and doses. Overall survival (OS) was defined from DLBCL diagnosis until time of death from any cause and differences in OS were determined by log-rank tests. Lymphoma-specific survival (LSS) was defined from DLBCL diagnosis until the time of death from DLBCL, with censoring occurring at the cause of death for causes other than DLBCL. To account for the impact of multiple variables on survival, a cox-regression model was implemented using the ‘stcox’ command. Differences in proportions for descriptive statistics were tested with a 2-sided Z-test. Data were interrogated to explore potential associations between route to diagnosis and baseline characteristics with OS and LSS.
Results
A total of 9186 DLBCL pts ≥65 years across a 3-year period (2013-2015) were identified. Median follow-up of the whole cohort was 2.1 years. 68% were aged 65-79 years. Gender distribution was equal. 4536 presented with stage III-IV (61%). Routes to initial diagnosis were emergency (34%), NHS urgent cancer referral pathway (29%) and standard GP referral (25%). The most common regimen was R-CHOP (n=4392), administered to 80.5% of those with a known regimen. 313 pts received R-miniCHOP (7% of all R-CHOP). For all pts, 3-year OS for those 65-79 years was 57% (95% confidence interval (CI) 56%>58%) and for ≥80 years was 32% (95% CI 30%>33%). 3-year OS for R-CHOP-treated pts diagnosed via emergency presentation (n=1160) was 54% (reference 1.00, GP referrals (Fig A): fully-adjusted hazard ratio (HR) 1.63 (95% CI:1.43-1.86, p<0.01) and 75% (fully-adjusted HR 0.81 (95% CI:0.71-0.93, p<0.01) on the NHS urgent cancer referral pathway (n=1635). NHS urgent cancer referral pathway retained its association with an improved LSS (HR 0.71, 95% CI 0.53-0.95, p=0.02), whilst pts with an emergency presentation had a significantly worse LSS by MVA (HR 1.95, 95% CI 1.49-2.54, p<0.01). 3-year OS was equivalent (54%) for both R-miniCHOP and R-CHOP in those ≥80 years (Fig B).
Conclusion
Our large, comprehensive real world practice analysis are the first to show that the NHS urgent cancer referral pathway leads to superior lymphoma-specific and overall survival in R-CHOP treated DLBCL pts even after adjusting for multiple confounders. Equivalent survival for R-CHOP and R-mini-CHOP in those ≥80 years supports the use of the latter in this setting.
Keyword(s):


