
Contributions
Abstract: EP494
Type: E-Poster Presentation
Session title: Acute myeloid leukemia - Clinical
Background
The management of acute myeloid leukemia (AML) in patients older than 60 years remains a major challenge as it is still rather unclear which patients will benefit or not from intensive chemotherapy compared to low intensity regimens according to clinical, molecular or cytogenetic markers. In relapse/refractory (R/r) settings, outcome in the elderly is usually very poor and there is currently no standard of care regarding second line or salvage therapy.
Aims
In this study, we aimed to investigate retrospectively the impact on the outcome of salvage/second line of treatment in R/r AML patients aged over 60 years old.
Methods
In this monocentric study, we analyzed 236 patients who were refractory to intensive (N=182) or semi-intensive (LIC) (low dose cytarabine/hypomethylating agents) (N=54) first line of treatment for newly diagnosed AML. Flow cytometry minimal residual disease (MRD) after intensive salvage chemotherapy was available in 42 patients and based on leukemia-associated immunophenotype (LAIP) using ELN recommendations (bulk lyses, and at least 500 000 live cells to achieve a sensitivity of 0.1%). MRD flow was performed in bone marrow samples using 8-color panel.
Results
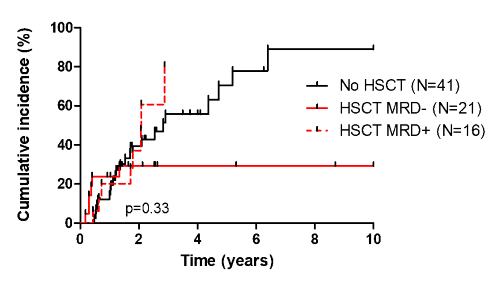
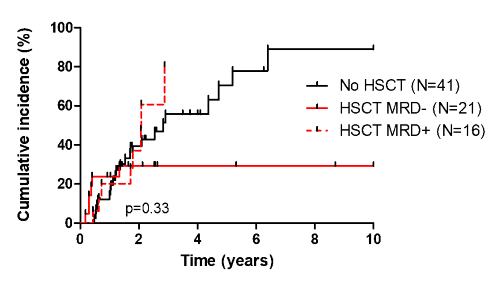
Overall, 50%, 24.6% and 25.4% of patients received either intensive (3+7 based), LIC or best supportive care (BSC) respectively. With a median follow-up of 15.2 months (range: 1.1-190), median overall survival (OS) of the entire cohort was 15.3 months. Median OS was 19.2, 21.6 and 14 months in patients receiving intensive salvage (N=118), LIC (N=58) and BSC (N=59) respectively (p=0.02). Regarding baseline characteristics at R/r, duration of 1st complete remission (CR) ELN 2013 classification and NPM1/FLT3-ITD status were predictive for long term survival. Median OS for NPM1+FLT3-, NPM1+FLT3-ITD and NPM1-FLT3-ITD was 25.4, 14.3 and 7 months respectively (p<0.001). Next generation sequencing at diagnosis was available in 83/237 patients. Median OS was higher in IDH1/2 mutated cases (46.8 months) compared to TP53, ASXL1/RUNX1 and MAPK/RTK mutated cases (p<0.001). Late relapse (LR) (defined as relapse occurring after 12 months after 1st CR) was associated with a better outcome independently of the treatment intensity compared to early relapse (ER)/refractory status. For intensively salvaged patients, CR and CRi/MLFS (according to ELN definition) was 21.2% and 23.7% respectively. Median OS was 34.9 and 21.2 months for CR and CRi/MLFS compared to 12.8 months in refractory patients (p<0.001). Post-induction MRD1 negativity (defined positive when ≥ 0.1%) for patients in CR2 was reached in 60.9% of cases. Among intensively salvaged patients, 20 received GO-based regimen. Sixty percent (12/20) of them reached CR2 (compared to 44.9% in non-GO based salvage, p=0.06). Cumulative incidence of relapse at 3 years was 49.1% and 77.5% in MRD1- and MRD1+ patients respectively. For those who underwent HSCT in CR2 (N=38), pre-HSCT MRD positivity was associated with a high rate of relapse which was similar to non-transplanted patients (figure). HSCT treatment related mortality was 31.5%.
Conclusion
These results suggest that intensive salvage chemotherapy might be preferred for patients eligible for HSCT in CR2. Post-intensive salvage MRD1 by flow cytometry might also identify patients with a more favorable outcome, even if HSCT seems to be detrimental for long term survival. Low intensive regimens might also be a suitable option in unfit and/or HSCT non-eligible patients, especially in the era of venetoclax and anti-IDH based regimens.
Keyword(s): AML, Elderly, Refractory, Relapse
Abstract: EP494
Type: E-Poster Presentation
Session title: Acute myeloid leukemia - Clinical
Background
The management of acute myeloid leukemia (AML) in patients older than 60 years remains a major challenge as it is still rather unclear which patients will benefit or not from intensive chemotherapy compared to low intensity regimens according to clinical, molecular or cytogenetic markers. In relapse/refractory (R/r) settings, outcome in the elderly is usually very poor and there is currently no standard of care regarding second line or salvage therapy.
Aims
In this study, we aimed to investigate retrospectively the impact on the outcome of salvage/second line of treatment in R/r AML patients aged over 60 years old.
Methods
In this monocentric study, we analyzed 236 patients who were refractory to intensive (N=182) or semi-intensive (LIC) (low dose cytarabine/hypomethylating agents) (N=54) first line of treatment for newly diagnosed AML. Flow cytometry minimal residual disease (MRD) after intensive salvage chemotherapy was available in 42 patients and based on leukemia-associated immunophenotype (LAIP) using ELN recommendations (bulk lyses, and at least 500 000 live cells to achieve a sensitivity of 0.1%). MRD flow was performed in bone marrow samples using 8-color panel.
Results
Overall, 50%, 24.6% and 25.4% of patients received either intensive (3+7 based), LIC or best supportive care (BSC) respectively. With a median follow-up of 15.2 months (range: 1.1-190), median overall survival (OS) of the entire cohort was 15.3 months. Median OS was 19.2, 21.6 and 14 months in patients receiving intensive salvage (N=118), LIC (N=58) and BSC (N=59) respectively (p=0.02). Regarding baseline characteristics at R/r, duration of 1st complete remission (CR) ELN 2013 classification and NPM1/FLT3-ITD status were predictive for long term survival. Median OS for NPM1+FLT3-, NPM1+FLT3-ITD and NPM1-FLT3-ITD was 25.4, 14.3 and 7 months respectively (p<0.001). Next generation sequencing at diagnosis was available in 83/237 patients. Median OS was higher in IDH1/2 mutated cases (46.8 months) compared to TP53, ASXL1/RUNX1 and MAPK/RTK mutated cases (p<0.001). Late relapse (LR) (defined as relapse occurring after 12 months after 1st CR) was associated with a better outcome independently of the treatment intensity compared to early relapse (ER)/refractory status. For intensively salvaged patients, CR and CRi/MLFS (according to ELN definition) was 21.2% and 23.7% respectively. Median OS was 34.9 and 21.2 months for CR and CRi/MLFS compared to 12.8 months in refractory patients (p<0.001). Post-induction MRD1 negativity (defined positive when ≥ 0.1%) for patients in CR2 was reached in 60.9% of cases. Among intensively salvaged patients, 20 received GO-based regimen. Sixty percent (12/20) of them reached CR2 (compared to 44.9% in non-GO based salvage, p=0.06). Cumulative incidence of relapse at 3 years was 49.1% and 77.5% in MRD1- and MRD1+ patients respectively. For those who underwent HSCT in CR2 (N=38), pre-HSCT MRD positivity was associated with a high rate of relapse which was similar to non-transplanted patients (figure). HSCT treatment related mortality was 31.5%.
Conclusion
These results suggest that intensive salvage chemotherapy might be preferred for patients eligible for HSCT in CR2. Post-intensive salvage MRD1 by flow cytometry might also identify patients with a more favorable outcome, even if HSCT seems to be detrimental for long term survival. Low intensive regimens might also be a suitable option in unfit and/or HSCT non-eligible patients, especially in the era of venetoclax and anti-IDH based regimens.
Keyword(s): AML, Elderly, Refractory, Relapse


