
Contributions
Abstract: EP489
Type: E-Poster Presentation
Session title: Acute myeloid leukemia - Clinical
Background
patients with Acute Myeloid Leukemia (AML) who achieve Complete Remission (CR) after 1 or 2 courses of chemotherapy need consolidation treatment to avoid relapse. We do not know what is the most effective chemotherapy scheme just after CR.
Aims
to analyse the impact of the first consolidation treatment (HDAC based, more intensive regimens including anthracyclines or directly transplant (HSCT) in terms of Relapse-Free Survival (RFS) and OS (OS) in patients with AML in CR after induction.
Methods
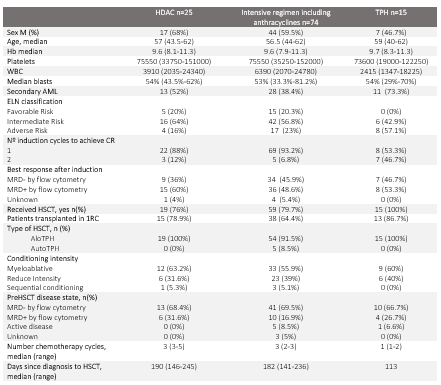
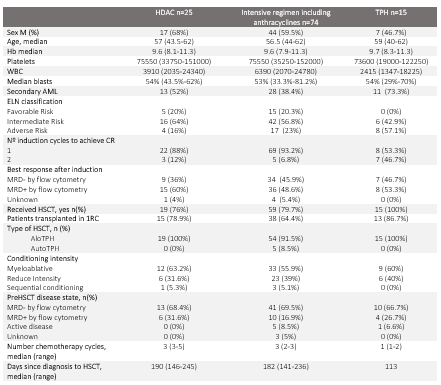
we reviewed retrospectively 190 patients with AML who were diagnosed between 2011 and 2020. We analysed 114 who achieve CR after 1 or 2 courses of intensive chemotherapy and received at least 1 cycle of consolidation or were directly transplanted after induction. We consider CR <5% blast by cytology and MRD+ ≥0.1% by Multiparameter Flow Cytometry (MFC). We divided the cohort according to the first consolidation treatment: Group 1 HDAC based consolidation, Group 2 intensive regimen including anthracyclines, and Group 3 HSCT directly HSCT. The decision on the first consolidation chemotherapy treatment (HDAC vs anthracyclines-based) was at the discretion of the prescribing physician. In table 1 are reflected the baselines characteristics of our cohort.
Results
we didn't find differences among the groups, except Group 3 had more percentage of secondary AML and adverse risk profile and they needed more frequently 2 cycles to achieve CR. With a median follow up of 19 months (12-47.5), the 3year (3y) EFS was 35%, the 3y-OS 45% and the 3y Cumulative Incidence of Relapse (3y-CIR) 43%. The 3y-EFS according to the first consolidation was 49% in Group 1 vs 30% Group 2 vs 39% in Group 3 (HR 1.2, p=0.2) and the 3y-OS was 54% Group1 vs 43% Group 2 vs 45% in Group 3 (HR 1.3, p=0.3). The CIR was 27% vs 49% vs 34% respectively (Grey test 3.2,p=0.2). Differences remained not significant after patients who received HSCT in CR were censored at the time of infusion for the EFS (HR 1.4, p=0.4). The response by both cytology and MFC before and after first consolidation were available in 21 HDAC-based first consolidation patients (9 MRD- after induction and 12 MRD+) and in 50 anthracycline-based first consolidation patients (25 MRD- and 25 MRD+). In patients with MRD- after induction, 1/9 patients had MRD+ and 1/9 patients had Active Disease (AD) after consolidation with HDAC and 1/25 patients had MRD+ and 1/25 AD after the consolidation with anthracyclines-based regimen (p=0.5). In patients with MRD+ after induction we found than in HDAC group, 3/12 patients achieve MRD- after the consolidation, 7/12 maintained MRD+ and 2/12 had AD while in anthracyclines-based first consolidation group, 13/25 patients achieved MRD-, 7/25 maintained MRD+ and 5/25 had AD (p=0.2). We analysed the impact of the first consolidation stratifying patients according to the MRD after induction (MRD+ and MRD-), the number of cycles (1 or 2) to achieve complete remission, the ELN at diagnosis (Favorable Intermediate and Adverse). We did not find statistical differences for EFS and OS according to the first consolidation in any of these subgroups.
Conclusion
the EFS and OS was not better using a first consolidation anthracycline-based compare to HDAC or patients that consolidate directly with HSCT regardless the MRD by flow cytometry after induction, the number of cycles to achieve CR or the cytogenetic risk. In patients with MRD+ after induction the first consolidation with another cycle of intensive chemotherapy based in anthracyclines did not significantly improve the depth of the response compare to standard HDAC regimen.
Keyword(s): Consolidation, Transplant
Abstract: EP489
Type: E-Poster Presentation
Session title: Acute myeloid leukemia - Clinical
Background
patients with Acute Myeloid Leukemia (AML) who achieve Complete Remission (CR) after 1 or 2 courses of chemotherapy need consolidation treatment to avoid relapse. We do not know what is the most effective chemotherapy scheme just after CR.
Aims
to analyse the impact of the first consolidation treatment (HDAC based, more intensive regimens including anthracyclines or directly transplant (HSCT) in terms of Relapse-Free Survival (RFS) and OS (OS) in patients with AML in CR after induction.
Methods
we reviewed retrospectively 190 patients with AML who were diagnosed between 2011 and 2020. We analysed 114 who achieve CR after 1 or 2 courses of intensive chemotherapy and received at least 1 cycle of consolidation or were directly transplanted after induction. We consider CR <5% blast by cytology and MRD+ ≥0.1% by Multiparameter Flow Cytometry (MFC). We divided the cohort according to the first consolidation treatment: Group 1 HDAC based consolidation, Group 2 intensive regimen including anthracyclines, and Group 3 HSCT directly HSCT. The decision on the first consolidation chemotherapy treatment (HDAC vs anthracyclines-based) was at the discretion of the prescribing physician. In table 1 are reflected the baselines characteristics of our cohort.
Results
we didn't find differences among the groups, except Group 3 had more percentage of secondary AML and adverse risk profile and they needed more frequently 2 cycles to achieve CR. With a median follow up of 19 months (12-47.5), the 3year (3y) EFS was 35%, the 3y-OS 45% and the 3y Cumulative Incidence of Relapse (3y-CIR) 43%. The 3y-EFS according to the first consolidation was 49% in Group 1 vs 30% Group 2 vs 39% in Group 3 (HR 1.2, p=0.2) and the 3y-OS was 54% Group1 vs 43% Group 2 vs 45% in Group 3 (HR 1.3, p=0.3). The CIR was 27% vs 49% vs 34% respectively (Grey test 3.2,p=0.2). Differences remained not significant after patients who received HSCT in CR were censored at the time of infusion for the EFS (HR 1.4, p=0.4). The response by both cytology and MFC before and after first consolidation were available in 21 HDAC-based first consolidation patients (9 MRD- after induction and 12 MRD+) and in 50 anthracycline-based first consolidation patients (25 MRD- and 25 MRD+). In patients with MRD- after induction, 1/9 patients had MRD+ and 1/9 patients had Active Disease (AD) after consolidation with HDAC and 1/25 patients had MRD+ and 1/25 AD after the consolidation with anthracyclines-based regimen (p=0.5). In patients with MRD+ after induction we found than in HDAC group, 3/12 patients achieve MRD- after the consolidation, 7/12 maintained MRD+ and 2/12 had AD while in anthracyclines-based first consolidation group, 13/25 patients achieved MRD-, 7/25 maintained MRD+ and 5/25 had AD (p=0.2). We analysed the impact of the first consolidation stratifying patients according to the MRD after induction (MRD+ and MRD-), the number of cycles (1 or 2) to achieve complete remission, the ELN at diagnosis (Favorable Intermediate and Adverse). We did not find statistical differences for EFS and OS according to the first consolidation in any of these subgroups.
Conclusion
the EFS and OS was not better using a first consolidation anthracycline-based compare to HDAC or patients that consolidate directly with HSCT regardless the MRD by flow cytometry after induction, the number of cycles to achieve CR or the cytogenetic risk. In patients with MRD+ after induction the first consolidation with another cycle of intensive chemotherapy based in anthracyclines did not significantly improve the depth of the response compare to standard HDAC regimen.
Keyword(s): Consolidation, Transplant


