
Contributions
Abstract: EP485
Type: E-Poster Presentation
Session title: Acute myeloid leukemia - Clinical
Background
Approximately 10% to 20% of patients with acute myeloid leukemia (AML) present with hyperleukocytosis. Hyperleukocytosis can result in leukostasis leading to end organ dysfunction and critical illness requiring admission to intensive care unit (ICU) admission. Institutional practices vary on the management of patients with hyperleukocytosis and leukostasis including location of chemotherapy administration and thresholds for ICU admission. There is paucity of data on the short- and long- term outcomes of these patients, particularly across those managed on in-patient wards compared to ICU.
Aims
To describe the characteristics of patients with hyperleukocytosis and factors associate with ICU admission and 60 day mortality.
Methods
We conducted a retrospective cohort study of consecutive admissions to Princess Margaret (PM) Cancer Center or Mount Sinai Hospital ICU between 2014-2019. All adult patients with a white blood cell count (WBC) >50x10^9/L and a new diagnosis of AML were included. Their clinical and laboratory data were evaluated across the first 5 days after presentation with hyperleukocytosis. Our primary outcome was ICU admission and our secondary outcome was 60 day mortality.
Results
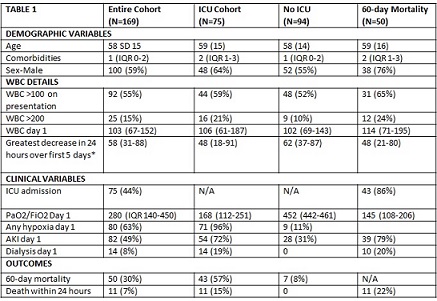
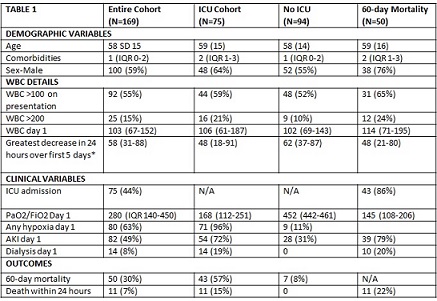
One-hundred and sixty-nine patients were admitted with a diagnosis of AML and hyperleukocytosis. Mean age was 58 (SD 15) and 59% were male with 43% having greater than 2 comorbidities. Median WBC on the first day of hyperleukocytosis was 103 x 10^9/L (IQR 67-152), with 55% having a WBC >100x10^9/L and 15% having a WBC >200x10^9/L. On the first day of hyperleukocytosis, 63% had hypoxemic respiratory failure, 25% had biochemical tumor lysis syndrome, and 49% were diagnosed with acute kidney injury (8% requiring dialysis) (Table 1). ICU admission was required in 44% of the cohort and the median time to ICU was 1 (IQR 0-3) day. Across entire cohort, median change in WBC from day 1 to 2 was – 17x10^9/L (IQR -31 - -1), the median greatest decrease in WBC over a 24 hour period was 58x10^9/L (31-88). Drop in WBC in first 5 days was higher in those not admitted to ICU and across survivors (Table 1). Across the ICU cohort, 59% required invasive mechanical ventilation, 76% had acute kidney injury and 48% require vasopressors. Across those admitted to the ICU, 81% were admitted within 4 days of hyperleukocytosis. Sixty-day mortality across the whole cohort was 30% (57% across the ICU cohort and 8% across the non-ICU exposed). ICU mortality was 82% across those who required invasive mechanical ventilation during the first 5 days post diagnosis of hyperleukocytosis. Hospital admission factors associated with ICU admission included hypoxia on day 1 of hyperleukocytosis (PaO2/FiO2 OR 0.97 (95% CI 0.96-0.98, p<0.001) and acute kidney injury (OR 12.2 95% CI 1.8-83, p 0.011). Factors associated with 60 day mortality included male sex, WBC >100x10^9/L, lower PaO2/FiO2, any invasive mechanical ventilation and a lower drop over a 24 hour period in the WBC across the first 5 days.
Conclusion
Patients with hyperleukocytosis managed on the inpatient wards had a mortality rate of 8%. Patients admitted to ICU and particularly those requiring invasive mechanical ventilation on admission had inferior survival.
Keyword(s): AML, Hyperleukocytosis
Abstract: EP485
Type: E-Poster Presentation
Session title: Acute myeloid leukemia - Clinical
Background
Approximately 10% to 20% of patients with acute myeloid leukemia (AML) present with hyperleukocytosis. Hyperleukocytosis can result in leukostasis leading to end organ dysfunction and critical illness requiring admission to intensive care unit (ICU) admission. Institutional practices vary on the management of patients with hyperleukocytosis and leukostasis including location of chemotherapy administration and thresholds for ICU admission. There is paucity of data on the short- and long- term outcomes of these patients, particularly across those managed on in-patient wards compared to ICU.
Aims
To describe the characteristics of patients with hyperleukocytosis and factors associate with ICU admission and 60 day mortality.
Methods
We conducted a retrospective cohort study of consecutive admissions to Princess Margaret (PM) Cancer Center or Mount Sinai Hospital ICU between 2014-2019. All adult patients with a white blood cell count (WBC) >50x10^9/L and a new diagnosis of AML were included. Their clinical and laboratory data were evaluated across the first 5 days after presentation with hyperleukocytosis. Our primary outcome was ICU admission and our secondary outcome was 60 day mortality.
Results
One-hundred and sixty-nine patients were admitted with a diagnosis of AML and hyperleukocytosis. Mean age was 58 (SD 15) and 59% were male with 43% having greater than 2 comorbidities. Median WBC on the first day of hyperleukocytosis was 103 x 10^9/L (IQR 67-152), with 55% having a WBC >100x10^9/L and 15% having a WBC >200x10^9/L. On the first day of hyperleukocytosis, 63% had hypoxemic respiratory failure, 25% had biochemical tumor lysis syndrome, and 49% were diagnosed with acute kidney injury (8% requiring dialysis) (Table 1). ICU admission was required in 44% of the cohort and the median time to ICU was 1 (IQR 0-3) day. Across entire cohort, median change in WBC from day 1 to 2 was – 17x10^9/L (IQR -31 - -1), the median greatest decrease in WBC over a 24 hour period was 58x10^9/L (31-88). Drop in WBC in first 5 days was higher in those not admitted to ICU and across survivors (Table 1). Across the ICU cohort, 59% required invasive mechanical ventilation, 76% had acute kidney injury and 48% require vasopressors. Across those admitted to the ICU, 81% were admitted within 4 days of hyperleukocytosis. Sixty-day mortality across the whole cohort was 30% (57% across the ICU cohort and 8% across the non-ICU exposed). ICU mortality was 82% across those who required invasive mechanical ventilation during the first 5 days post diagnosis of hyperleukocytosis. Hospital admission factors associated with ICU admission included hypoxia on day 1 of hyperleukocytosis (PaO2/FiO2 OR 0.97 (95% CI 0.96-0.98, p<0.001) and acute kidney injury (OR 12.2 95% CI 1.8-83, p 0.011). Factors associated with 60 day mortality included male sex, WBC >100x10^9/L, lower PaO2/FiO2, any invasive mechanical ventilation and a lower drop over a 24 hour period in the WBC across the first 5 days.
Conclusion
Patients with hyperleukocytosis managed on the inpatient wards had a mortality rate of 8%. Patients admitted to ICU and particularly those requiring invasive mechanical ventilation on admission had inferior survival.
Keyword(s): AML, Hyperleukocytosis


