
Contributions
Abstract: EP475
Type: E-Poster Presentation
Session title: Acute myeloid leukemia - Clinical
Background
Newly-diagnosed acute myeloid leukemia (NDAML) patients (pts) frequently develop catheter-related thrombosis (CRT) despite concurrent thrombocytopenia. The risk of symptomatic CRT in these pts varies between 5%>10%. While risk factors for CRT occurrence in pts with solid tumors are well-established, such data in NDAML are scarce. CRT treatment in NDAML is challenging due to concomitant severe thrombocytopenia and high bleeding risk. Current treatment strategies include catheter removal and full/low dose anticoagulation supported by platelet transfusion. Modification of anticoagulant therapy is based on platelet counts, with predetermined cutoffs for dose adjustment (25-50x109) and treatment cessation (<25x109).
Aims
We aimed to identify risk factors for CRT development in NDAML and to assess the efficacy of anticoagulation [low molecular weight heparin (LMWH)] along with its complications.
Methods
This retrospective analysis included all consecutive pts treated at the Rambam Health Care Campus between 2006-2019 for NDAML using a central venous catheter (CVC). Data on patient demographics, clinical characteristics, lab results and vital signs at diagnosis were automatically collected using a designated big-data platform (MDClone, Beer-Sheba, Israel). Intensity of CRT treatment and related bleeding complications were recorded along with the rate of venous thromboembolism (VTE) recurrence. Rates or proportions were compared using t-test or Wilcoxon test for continuous variables, and Chi-square test or Fisher's exact test for categorical variables. A multivariable logistic regression analysis was performed.
Results
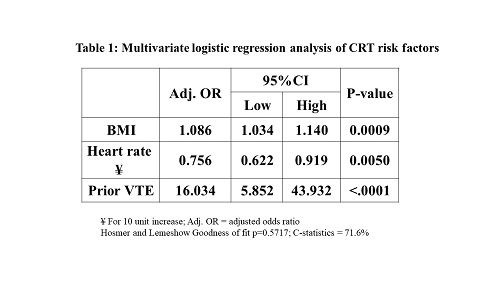
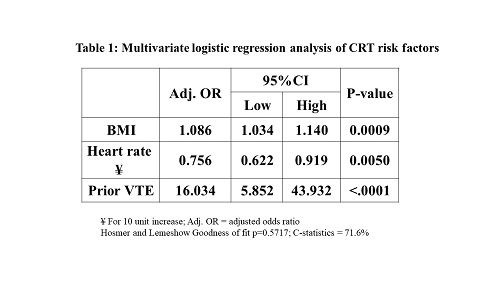
Out of 632 evaluable NDAML pts 64 (10.1%) developed CRT. In a univariate analysis, the following CRT risk factors were identified: AML subtype [non-acute promyelocytic leukemia (non-APL) vs. APL, OR 0.39; 95%CI 0.17-0.86; p=0.02)], BMI (OR 1.05; 95%CI 1.01-1.10; p=0.01), heart rate at diagnosis (OR 0.76; 95%CI 0.63-0.91; p=0.003), and history of prior VTE (OR 16.87; 95%CI 5.33-53.41; p<0.001). In multivariate analysis, BMI, heart rate and history of prior VTE provided a good prediction model (C-Statistic 71.6%) (Table 1). While pts with CRT had lower platelet levels at diagnosis (107000; SD 148000 vs. 146000; SD 139; p=0.003), this parameter was found to be a poor CRT predictor (ROC curve area-under-curve 61.4%; 95%CI 54.1%>68.7%). The CVC was removed in 51 (80%) of 64 pts, which was in most cases associated with catheter-related bloodstream infection (p=0.050). Pts treated with full-dose LMWH were more likely to suffer from gastrointestinal bleed than those receiving reduced dose or no anticoagulant at all (p=0.003). There was no significant difference in blood products use before or after CRT-related anticoagulant treatment initiation (blood product per week per each patient). The lack of correlation between CRT or anticoagulation and blood product use could be explained by other medical conditions requiring blood transfusion (e.g., symptomatic anemia, severe thrombocytopenia).
At a mean follow-up of 2.9 years, CRT recurrence was recorded in 8 pts (12.5%). There was no difference in CRT recurrence between pts treated with different anticoagulant doses (p=0.40).
Conclusion
In this large cohort of NDAML patients treated at a tertiary care center, BMI, heart rate and history of prior VTE emerged as significant CRT risk factors. Neither complete blood count nor platelet levels were found to be reliable CRT predictors. Importantly, platelet count-based modification of anticoagulation dose appeared to be efficacious and relatively safe.
Keyword(s): Acute myeloid leukemia, Central venous catheter, Thrombosis
Abstract: EP475
Type: E-Poster Presentation
Session title: Acute myeloid leukemia - Clinical
Background
Newly-diagnosed acute myeloid leukemia (NDAML) patients (pts) frequently develop catheter-related thrombosis (CRT) despite concurrent thrombocytopenia. The risk of symptomatic CRT in these pts varies between 5%>10%. While risk factors for CRT occurrence in pts with solid tumors are well-established, such data in NDAML are scarce. CRT treatment in NDAML is challenging due to concomitant severe thrombocytopenia and high bleeding risk. Current treatment strategies include catheter removal and full/low dose anticoagulation supported by platelet transfusion. Modification of anticoagulant therapy is based on platelet counts, with predetermined cutoffs for dose adjustment (25-50x109) and treatment cessation (<25x109).
Aims
We aimed to identify risk factors for CRT development in NDAML and to assess the efficacy of anticoagulation [low molecular weight heparin (LMWH)] along with its complications.
Methods
This retrospective analysis included all consecutive pts treated at the Rambam Health Care Campus between 2006-2019 for NDAML using a central venous catheter (CVC). Data on patient demographics, clinical characteristics, lab results and vital signs at diagnosis were automatically collected using a designated big-data platform (MDClone, Beer-Sheba, Israel). Intensity of CRT treatment and related bleeding complications were recorded along with the rate of venous thromboembolism (VTE) recurrence. Rates or proportions were compared using t-test or Wilcoxon test for continuous variables, and Chi-square test or Fisher's exact test for categorical variables. A multivariable logistic regression analysis was performed.
Results
Out of 632 evaluable NDAML pts 64 (10.1%) developed CRT. In a univariate analysis, the following CRT risk factors were identified: AML subtype [non-acute promyelocytic leukemia (non-APL) vs. APL, OR 0.39; 95%CI 0.17-0.86; p=0.02)], BMI (OR 1.05; 95%CI 1.01-1.10; p=0.01), heart rate at diagnosis (OR 0.76; 95%CI 0.63-0.91; p=0.003), and history of prior VTE (OR 16.87; 95%CI 5.33-53.41; p<0.001). In multivariate analysis, BMI, heart rate and history of prior VTE provided a good prediction model (C-Statistic 71.6%) (Table 1). While pts with CRT had lower platelet levels at diagnosis (107000; SD 148000 vs. 146000; SD 139; p=0.003), this parameter was found to be a poor CRT predictor (ROC curve area-under-curve 61.4%; 95%CI 54.1%>68.7%). The CVC was removed in 51 (80%) of 64 pts, which was in most cases associated with catheter-related bloodstream infection (p=0.050). Pts treated with full-dose LMWH were more likely to suffer from gastrointestinal bleed than those receiving reduced dose or no anticoagulant at all (p=0.003). There was no significant difference in blood products use before or after CRT-related anticoagulant treatment initiation (blood product per week per each patient). The lack of correlation between CRT or anticoagulation and blood product use could be explained by other medical conditions requiring blood transfusion (e.g., symptomatic anemia, severe thrombocytopenia).
At a mean follow-up of 2.9 years, CRT recurrence was recorded in 8 pts (12.5%). There was no difference in CRT recurrence between pts treated with different anticoagulant doses (p=0.40).
Conclusion
In this large cohort of NDAML patients treated at a tertiary care center, BMI, heart rate and history of prior VTE emerged as significant CRT risk factors. Neither complete blood count nor platelet levels were found to be reliable CRT predictors. Importantly, platelet count-based modification of anticoagulation dose appeared to be efficacious and relatively safe.
Keyword(s): Acute myeloid leukemia, Central venous catheter, Thrombosis


