
Contributions
Abstract: EP434
Type: E-Poster Presentation
Session title: Acute myeloid leukemia - Clinical
Background
The connotation surrounding AML is often grim because of the heightened risk of mortality within the first few years post-diagnosis. Therefore, survival estimates measured from diagnosis, which is usually presented in population-based cancer research, might be somewhat pessimistic for long-term AML survivors and their caregivers who desire to obtain information on the prognosis after having survived some years post-diagnosis.
Aims
Against this background, this population-based study aimed to estimate the conditional 5-year relative survival among AML patients up to 15 years post-diagnosis.
Methods
All adult (≥18 years) AML patients diagnosed between 1989-2018—with follow-up for survival through December 31, 2019—were selected from the Netherlands Cancer Registry. We excluded patients with acute promyelocytic leukemia. Relative survival (RS) was calculated to estimate disease-specific survival as the ratio of the observed to the expected survival, based on national life tables stratified by age, sex, and calendar year. We computed 5-year RS at diagnosis and for each additional year survived up to 15 years post-diagnosis. RS was estimated using a hybrid approach to predict up-to-date survival probabilities. This approach was applied for patients diagnosed between 1989-2018 who were alive during the follow-up interval 2008-2019. The produced estimates can be interpreted as the predicted survival probability of patients diagnosed during 2008-2019. Survival estimates were computed—with associated 95% confidence intervals (CIs)—according to age at diagnosis (18-40, 41-60, 61-70, and >70 years). Only survival estimates with a standard error of ≤5% were presented. This choice relates to the precision of the survival estimates. Excess mortality is minimal when RS is ≥95%.
Results
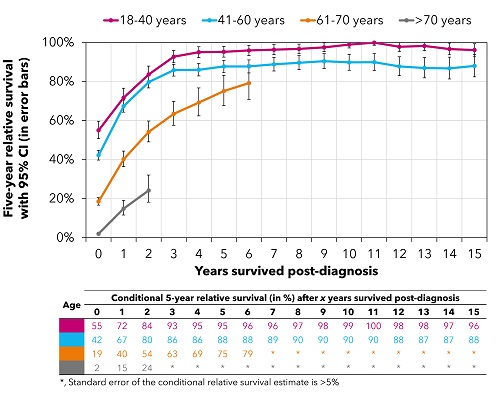
A total of 16,177 adult AML patients (median age, 68 years) were diagnosed in the Netherlands between 1989-2018, of whom 8,182 (51%) were alive at some point during the follow-up interval and contributed to the survival estimates. There was a prognostic effect of age on 5-year RS at diagnosis, with corresponding estimates (95% CI) of 55% (51% - 60%), 42% (40% - 45%), 19% (17% - 21%), and 2% (2% - 3%) across the four age groups (Figure). This effect essentially persisted up to 15 years post-diagnosis (Figure). Notwithstanding, excess mortality decreased with each additional year survived across all age groups (Figure). Encouragingly enough, patients aged 18-40 years at diagnosis hardly experienced excess mortality after four years post-diagnosis (Figure). In contrast, excess mortality remained substantial for patients aged >40 years, especially among those aged >60 years (Figure).
Conclusion
The prognosis of adult AML patients improved with each additional year survived. Reassuring is that patients aged 18-40 years at diagnosis can look forward to a near-normal life expectancy after four year post-diagnosis. This finding, unfortunately, does not hold for patients aged >40 years at diagnosis. Late treatment-related sequelae and late relapses might cause the ongoing excess mortality among patients aged 41-70 years, a group mostly considered for intensive, potentially curative treatment. The poor outcome among patients aged >70 years is inherently tied to the virtually incurable nature of AML in this age group. Statistics on CRS in AML may offer patients and physicians a better apprehension of the changing survival expectations with each additional year survived post-diagnosis. This information can also be used to tailor age-specific surveillance and follow-up activities.
Keyword(s): Acute myeloid leukemia, Epidemiology, Population, Survival
Abstract: EP434
Type: E-Poster Presentation
Session title: Acute myeloid leukemia - Clinical
Background
The connotation surrounding AML is often grim because of the heightened risk of mortality within the first few years post-diagnosis. Therefore, survival estimates measured from diagnosis, which is usually presented in population-based cancer research, might be somewhat pessimistic for long-term AML survivors and their caregivers who desire to obtain information on the prognosis after having survived some years post-diagnosis.
Aims
Against this background, this population-based study aimed to estimate the conditional 5-year relative survival among AML patients up to 15 years post-diagnosis.
Methods
All adult (≥18 years) AML patients diagnosed between 1989-2018—with follow-up for survival through December 31, 2019—were selected from the Netherlands Cancer Registry. We excluded patients with acute promyelocytic leukemia. Relative survival (RS) was calculated to estimate disease-specific survival as the ratio of the observed to the expected survival, based on national life tables stratified by age, sex, and calendar year. We computed 5-year RS at diagnosis and for each additional year survived up to 15 years post-diagnosis. RS was estimated using a hybrid approach to predict up-to-date survival probabilities. This approach was applied for patients diagnosed between 1989-2018 who were alive during the follow-up interval 2008-2019. The produced estimates can be interpreted as the predicted survival probability of patients diagnosed during 2008-2019. Survival estimates were computed—with associated 95% confidence intervals (CIs)—according to age at diagnosis (18-40, 41-60, 61-70, and >70 years). Only survival estimates with a standard error of ≤5% were presented. This choice relates to the precision of the survival estimates. Excess mortality is minimal when RS is ≥95%.
Results
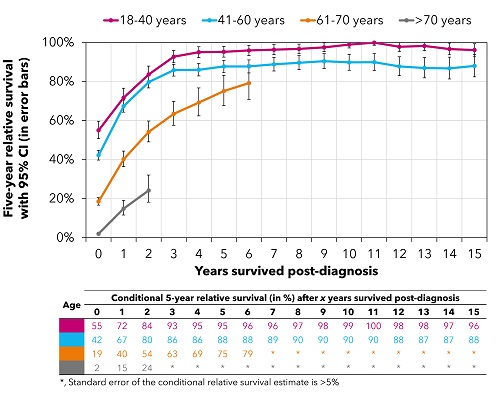
A total of 16,177 adult AML patients (median age, 68 years) were diagnosed in the Netherlands between 1989-2018, of whom 8,182 (51%) were alive at some point during the follow-up interval and contributed to the survival estimates. There was a prognostic effect of age on 5-year RS at diagnosis, with corresponding estimates (95% CI) of 55% (51% - 60%), 42% (40% - 45%), 19% (17% - 21%), and 2% (2% - 3%) across the four age groups (Figure). This effect essentially persisted up to 15 years post-diagnosis (Figure). Notwithstanding, excess mortality decreased with each additional year survived across all age groups (Figure). Encouragingly enough, patients aged 18-40 years at diagnosis hardly experienced excess mortality after four years post-diagnosis (Figure). In contrast, excess mortality remained substantial for patients aged >40 years, especially among those aged >60 years (Figure).
Conclusion
The prognosis of adult AML patients improved with each additional year survived. Reassuring is that patients aged 18-40 years at diagnosis can look forward to a near-normal life expectancy after four year post-diagnosis. This finding, unfortunately, does not hold for patients aged >40 years at diagnosis. Late treatment-related sequelae and late relapses might cause the ongoing excess mortality among patients aged 41-70 years, a group mostly considered for intensive, potentially curative treatment. The poor outcome among patients aged >70 years is inherently tied to the virtually incurable nature of AML in this age group. Statistics on CRS in AML may offer patients and physicians a better apprehension of the changing survival expectations with each additional year survived post-diagnosis. This information can also be used to tailor age-specific surveillance and follow-up activities.
Keyword(s): Acute myeloid leukemia, Epidemiology, Population, Survival


