
Contributions
Abstract: EP368
Type: E-Poster Presentation
Session title: Acute lymphoblastic leukemia - Clinical
Background
Acute lymphoblastic leukemia (ALL) is the most common type of leukemia in children. However, the epidemiology, treatment patterns, and clinical outcomes of pediatric ALL in Asian population are still limited.
Aims
To investigate the incidence of ALL in pediatric population and their baseline characteristics, treatment patterns as well as clinical outcomes in Taiwan.
Methods
We conducted a nationwide population-based retrospective cohort study using the Taiwan Cancer Registry (TCR) and National Health Insurance Research Database (NHIRD). In the first part of our analysis, pediatric patients newly diagnosed with ALL from 2002 to 2017 were identified from the TCR and the annual incidence of ALL were reported. In the second part of our analysis, we further focused on the pediatric patients diagnosed with B-cell ALL during 2009 to 2015 and investigated their baseline characteristics, treatment patterns and clinical outcomes. Outcomes of interest included refractory disease, disease relapse and all cause mortality. Kaplan-Meier survival analysis were performed with stratification by induction therapy or not, age at diagnosis and response of induction therapy.
Results
The annual incidence of ALL in pediatric population ranged from 2.36 to 3.19 cases per 100,000 persons, with the highest incidence in the age group of 1 to 4 years. Mean age at diagnosis was 7.1 years.
Among 787 pediatric patients with B-cell ALL identified in TCRD, 761 (96.7%) patients received their induction therapy within 4 months after diagnosis of ALL and were identified for further analysis. Their median age ranged from 3 to 5 years old in the different fiscal year. Most of the patients (97.4 %) were treated in a medical center and initiated induction therapy within the first week after diagnosis, with median time internval ranging from 0 to 7 days.
The proportion of the patients who achieved remission state increased steadily over the years and achieved 97.0% in 2015. In patients who achieved remission state, approximately 20% of them encountered relapse. The cumulative mortality were 26.4% in 2009 and 8.0% in 2015. The proportion of patients received stem cell transplantation (SCT) were 11.2% in 2009 and 7.0% in 2015.
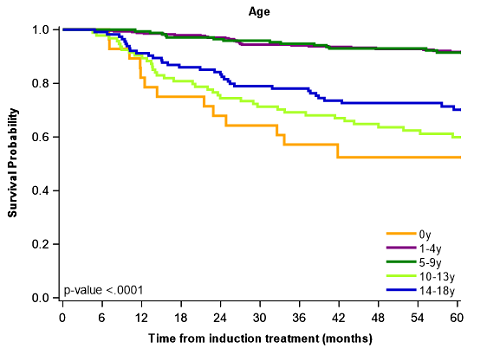
As for the survival analysis, the 3-year survival rate is 87% in patients with induction therapy, with best 3-year survival rate of 94% and 95% in age groups of 1 to 4 and 5 to 9.
The survival of patients who received induction therapy were significantly better than those who did not. The survival were also significantly different in different age at diagnosis, with age groups ranging from 1 to 4 and 5 to 9 having the best survival. Patients who did not encountered refractory disease also showed better survival. Similar trend were observed in relapse-free survival, with better survival in age group 1 to 4 and 5 to 9.
Conclusion
Our study, with the advantage of 16 years of longitudinal data, has provided epidemiology, treatment patterns and survivals of pediatric ALL in the past decades in Taiwan. The annual incidence of ALL were approximately 2.8 per 100,000 person in Taiwanese pediatric population, with the highest incidence in the age group of 1 to 4 years. Most of the patients achieved remission state after induction therapy, of whom approximately 20% encountered relapse. The 3-year survival rate is 87% in patients with induction therapy. Best survival were observed in the age groups of 1 to 4 and 5 to 9, with 3-year survival rate of 94% and 95%.
Keyword(s):
Abstract: EP368
Type: E-Poster Presentation
Session title: Acute lymphoblastic leukemia - Clinical
Background
Acute lymphoblastic leukemia (ALL) is the most common type of leukemia in children. However, the epidemiology, treatment patterns, and clinical outcomes of pediatric ALL in Asian population are still limited.
Aims
To investigate the incidence of ALL in pediatric population and their baseline characteristics, treatment patterns as well as clinical outcomes in Taiwan.
Methods
We conducted a nationwide population-based retrospective cohort study using the Taiwan Cancer Registry (TCR) and National Health Insurance Research Database (NHIRD). In the first part of our analysis, pediatric patients newly diagnosed with ALL from 2002 to 2017 were identified from the TCR and the annual incidence of ALL were reported. In the second part of our analysis, we further focused on the pediatric patients diagnosed with B-cell ALL during 2009 to 2015 and investigated their baseline characteristics, treatment patterns and clinical outcomes. Outcomes of interest included refractory disease, disease relapse and all cause mortality. Kaplan-Meier survival analysis were performed with stratification by induction therapy or not, age at diagnosis and response of induction therapy.
Results
The annual incidence of ALL in pediatric population ranged from 2.36 to 3.19 cases per 100,000 persons, with the highest incidence in the age group of 1 to 4 years. Mean age at diagnosis was 7.1 years.
Among 787 pediatric patients with B-cell ALL identified in TCRD, 761 (96.7%) patients received their induction therapy within 4 months after diagnosis of ALL and were identified for further analysis. Their median age ranged from 3 to 5 years old in the different fiscal year. Most of the patients (97.4 %) were treated in a medical center and initiated induction therapy within the first week after diagnosis, with median time internval ranging from 0 to 7 days.
The proportion of the patients who achieved remission state increased steadily over the years and achieved 97.0% in 2015. In patients who achieved remission state, approximately 20% of them encountered relapse. The cumulative mortality were 26.4% in 2009 and 8.0% in 2015. The proportion of patients received stem cell transplantation (SCT) were 11.2% in 2009 and 7.0% in 2015.
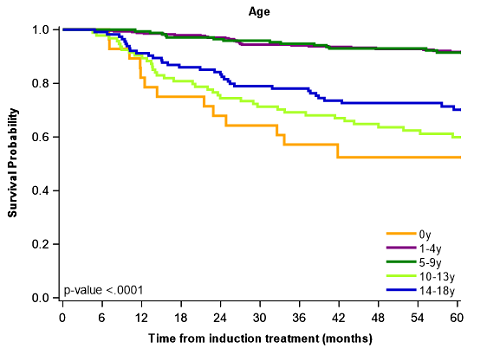
As for the survival analysis, the 3-year survival rate is 87% in patients with induction therapy, with best 3-year survival rate of 94% and 95% in age groups of 1 to 4 and 5 to 9.
The survival of patients who received induction therapy were significantly better than those who did not. The survival were also significantly different in different age at diagnosis, with age groups ranging from 1 to 4 and 5 to 9 having the best survival. Patients who did not encountered refractory disease also showed better survival. Similar trend were observed in relapse-free survival, with better survival in age group 1 to 4 and 5 to 9.
Conclusion
Our study, with the advantage of 16 years of longitudinal data, has provided epidemiology, treatment patterns and survivals of pediatric ALL in the past decades in Taiwan. The annual incidence of ALL were approximately 2.8 per 100,000 person in Taiwanese pediatric population, with the highest incidence in the age group of 1 to 4 years. Most of the patients achieved remission state after induction therapy, of whom approximately 20% encountered relapse. The 3-year survival rate is 87% in patients with induction therapy. Best survival were observed in the age groups of 1 to 4 and 5 to 9, with 3-year survival rate of 94% and 95%.
Keyword(s):


