
Contributions
Abstract: EP361
Type: E-Poster Presentation
Session title: Acute lymphoblastic leukemia - Clinical
Background
Measurable residual disease (MRD) is an independent prognostic factor in numerous acute lymphoblastic leukemia (ALL) studies. An unfavorable outcome may be dependent not only on the persistence of MRD, but on immunophenotype of residual blasts too. Immunophenotype could reflect the biology of tumor cells, especially their genetics (Gupta N. et al., 2019).
Aims
The aim was to investigate a significance of MRD and immunophenotype of residual blasts at the end of induction in Russian treatment protocol RALL-2016.
Methods
The multicenter study RALL-2016 (NCT03462095) included 207 adult patients from 2016 to 2020 years. The MRD was assessed at the end of induction (day 70) in 150 patients (80 patients with B-ALL and 70 patients with T-ALL) who achieved a complete remission. Analysis of MRD was performed in the bone marrow samples by flow cytometer instruments FACSCanto II (Becton Dickinson) or CytoFLEX (Beckman Coulter). The sensitivity was at least 0.01%. Seven basic antigens (CD19, CD34, CD10, CD20, CD38, CD45 and CD58) were analyzed to detect MRD and were used to describe the immunophenotype of residual blasts in B-ALL at day 70. The relative expression of these antigens was determined compared to normal cells of bone marrow (Dworzak M.N. et al., 2017) and translated into numerical equivalent as it was described earlier (Davydova Y. et al, HemaSpere – materials of EHA 2020). A dendrogram was constructed using the “ward.D2” method in R 3.4.4. The probability of relapse-free survival (RFS) was estimated with the Kaplan–Meier method, and comparisons were assessed using the log-rank test. A p < 0.05 was considered significant.
Results
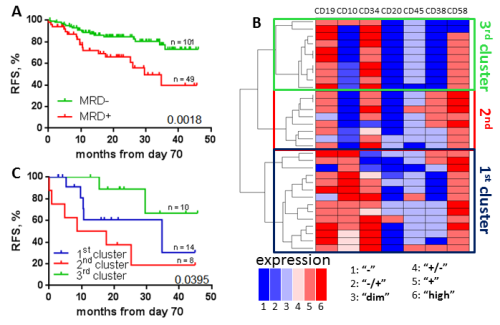
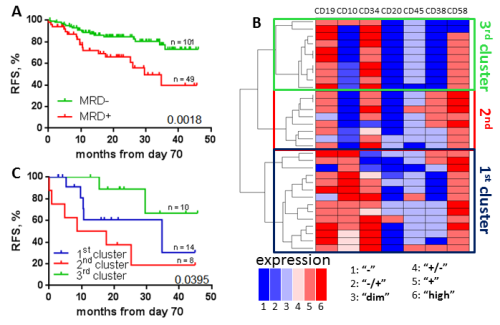
At the end of induction 101 (67.3%) patients (48 B-ALL, and 53 T-ALL) were MRD-negative, and 49 (32.7%) patients (32 B-ALL, and 17 T-ALL) remained residual blasts. RFS was higher in MRD-negative than in MRD-positive patients (median undefined vs 29.5 months, p=0.002) in whole ALL cohort (fig. A). Analyzing B-ALL cohort, the RFS was depended on MRD (median undefined vs 29.5 months, p=0.004), but in T-ALL MRD was not significant (medians undefined, p=0.25).
Cluster analysis revealed 3 clusters in B-ALL MRD based on immunophenotype of residual blasts (fig. B). The 1st cluster (n=14) included cases with presence of CD10 while 2nd (n=8), and 3rd (n=10) clusters included CD10-negative cases. The expression of CD38, and CD58 was higher in 2nd than in 3rd cluster.
RFS probability differed in these 3 clusters: medians were 34.7 months, 13.1 months, and undefined in 1st, 2nd, and 3rd clusters, respectively (p=0.04) (Fig.C).
Conclusion
MRD measured by flow cytometry at the end of induction was confirmed as an important prognostic factor in RALL-2016 protocol among B-ALL patients. Immunophenotype of residual blasts was in association with the RFS. The most unfavorable prognosis was in cases that lack CD10 expression but have relatively high expression of CD58, and CD38.
Keyword(s): Acute lymphoblastic leukemia, Flow cytometry, Immunophenotype, Minimal residual disease (MRD)
Abstract: EP361
Type: E-Poster Presentation
Session title: Acute lymphoblastic leukemia - Clinical
Background
Measurable residual disease (MRD) is an independent prognostic factor in numerous acute lymphoblastic leukemia (ALL) studies. An unfavorable outcome may be dependent not only on the persistence of MRD, but on immunophenotype of residual blasts too. Immunophenotype could reflect the biology of tumor cells, especially their genetics (Gupta N. et al., 2019).
Aims
The aim was to investigate a significance of MRD and immunophenotype of residual blasts at the end of induction in Russian treatment protocol RALL-2016.
Methods
The multicenter study RALL-2016 (NCT03462095) included 207 adult patients from 2016 to 2020 years. The MRD was assessed at the end of induction (day 70) in 150 patients (80 patients with B-ALL and 70 patients with T-ALL) who achieved a complete remission. Analysis of MRD was performed in the bone marrow samples by flow cytometer instruments FACSCanto II (Becton Dickinson) or CytoFLEX (Beckman Coulter). The sensitivity was at least 0.01%. Seven basic antigens (CD19, CD34, CD10, CD20, CD38, CD45 and CD58) were analyzed to detect MRD and were used to describe the immunophenotype of residual blasts in B-ALL at day 70. The relative expression of these antigens was determined compared to normal cells of bone marrow (Dworzak M.N. et al., 2017) and translated into numerical equivalent as it was described earlier (Davydova Y. et al, HemaSpere – materials of EHA 2020). A dendrogram was constructed using the “ward.D2” method in R 3.4.4. The probability of relapse-free survival (RFS) was estimated with the Kaplan–Meier method, and comparisons were assessed using the log-rank test. A p < 0.05 was considered significant.
Results
At the end of induction 101 (67.3%) patients (48 B-ALL, and 53 T-ALL) were MRD-negative, and 49 (32.7%) patients (32 B-ALL, and 17 T-ALL) remained residual blasts. RFS was higher in MRD-negative than in MRD-positive patients (median undefined vs 29.5 months, p=0.002) in whole ALL cohort (fig. A). Analyzing B-ALL cohort, the RFS was depended on MRD (median undefined vs 29.5 months, p=0.004), but in T-ALL MRD was not significant (medians undefined, p=0.25).
Cluster analysis revealed 3 clusters in B-ALL MRD based on immunophenotype of residual blasts (fig. B). The 1st cluster (n=14) included cases with presence of CD10 while 2nd (n=8), and 3rd (n=10) clusters included CD10-negative cases. The expression of CD38, and CD58 was higher in 2nd than in 3rd cluster.
RFS probability differed in these 3 clusters: medians were 34.7 months, 13.1 months, and undefined in 1st, 2nd, and 3rd clusters, respectively (p=0.04) (Fig.C).
Conclusion
MRD measured by flow cytometry at the end of induction was confirmed as an important prognostic factor in RALL-2016 protocol among B-ALL patients. Immunophenotype of residual blasts was in association with the RFS. The most unfavorable prognosis was in cases that lack CD10 expression but have relatively high expression of CD58, and CD38.
Keyword(s): Acute lymphoblastic leukemia, Flow cytometry, Immunophenotype, Minimal residual disease (MRD)


