
Contributions
Abstract: EP359
Type: E-Poster Presentation
Session title: Acute lymphoblastic leukemia - Clinical
Background
Survival after allogeneic hematopoietic cell transplantation (HCT) of high-risk acute lymphoblastic leukemia (ALL) is challenged by high risk of relapse and non-relapse mortality (NRM) due to conditioning toxicity or graft-versus-host disease (GvHD).
Aims
We aimed to investigate temporal trends of survival in a nationwide population-based cohort study of adults (≥18 years) who received HCT for ALL in Denmark between 2000–2019.
Methods
Indications for HCT comprised high-risk ALL (including Philadelphia chromosome positive [Ph+] ALL) or ALL in >1st complete remission (CR). From 2011, non-myeloablative HCT was perfomed for patients >50 years or with comorbidities, and from 2012, Ph+ patients received a tyrosine kinase inhibitor one year post-HCT. Temporal trends in overall survival (OS) were examined in a Royston–Parmar survival model. A non-mixture cure model was used to estimate temporal trends in short- and long-term survival, respectively (long-term survival estimated as the cure fraction, i.e. the fraction of patients who experienced no excess mortality compared to the Danish general population matched on calendar year, age and sex). Hazard ratios (HR) of relapse and NRM were estimated in cause-specific Cox models. Cumulative incidences of HCT outcomes were calculated by the Aalen-Johansen method and compared between patients transplanted in the earliest vs. latest quartile (years 2000–2005 vs. 2016–2019).
Results
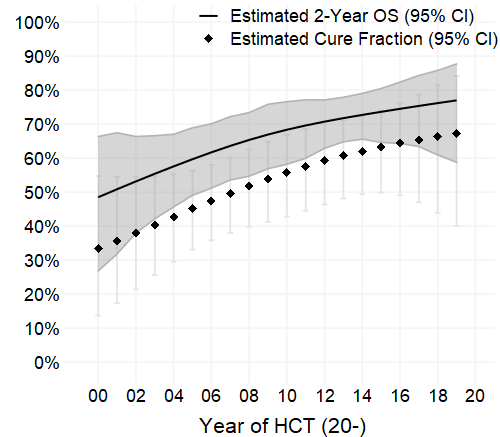
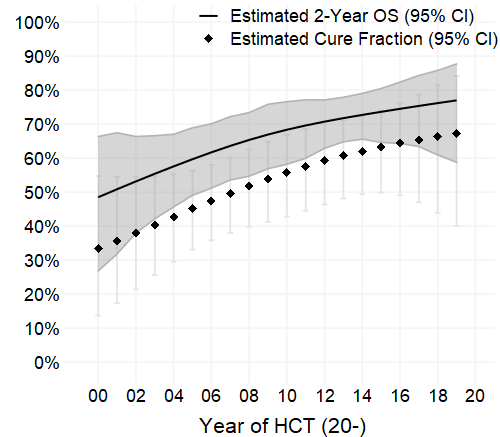
From 2000 to 2019, 181 adults were transplanted for ALL in Denmark; 83% with B-cell, 17% with T-cell and 31% with Ph+ ALL. Median (min–max) age at transplant was 36 (18–74) years. Most patients (72%) were transplanted in CR1, and the median time from diagnosis to transplant was 7 months. The most common regimen was myeloablative (84%) transplant (Eto- or CyTBI) with a matched unrelated donor (56%). In later time periods, more patients were transplanted in CR1 and with non-myeloablative conditioning, while the proportion of patients with Ph+ ALL was constant. At a median follow-up of 8.1 years, 77 (43%) patients had died. The 2- and 5-year Kaplan–Meier OS (95% CI) were 69% (63%, 76%) and 62% (55%, 70%) in the entire cohort. OS increased with year of HCT (p = 0.03) with an estimated 2-year OS (95% CI) of 49% (27%, 66%) in patients transplanted in year 2000 vs. 77% (59%, 88%) in 2019 (Figure). The estimated cure fraction increased over time (odds ratio for cure per calendar year increase: 1.08; 95% CI: 1.01, 1.15; p = 0.03), whereas the short-term excess hazard of dying did not change significantly (HR per calendar year: 1.00; 95% CI: 0.93, 1.07; p = 0.97). This was reflected in the decreased risk of relapse over time (HR 0.92 per calendar year; 95% CI: 0.87, 0.98, p = 0.01; 2-year cumulative incidence in years 2000–2005: 26% [95% CI: 12%, 39%] vs. 12% [95% CI: 3%, 21%] in years 2016–2019), and the stable risk of NRM (HR 0.98 per calendar year; 95% CI: 0.93, 1.04, p = 0.49; 2-year cumulative incidence in years 2000–2005: 21% [95% CI: 9%, 33%] vs. 16% [95% CI: 6%, 26%] in years 2016–2019). The incidence of GvHD did not change markedly over time (grade II–IV acute GvHD: 35% [95% CI: 20%, 49%] in years 2000–2005 vs. 37% [95% CI: 24%, 51%] in years 2016–2019; chronic GvHD at 2 years: 40% [95% CI: 25%, 54%] in years 2000–2005 vs. 51% [95% CI: 37%, 65%] in years 2016–2019).
Conclusion
In a nationwide cohort study of HCT-treated ALL-patients, we found an improved long-term survival from 2000 to 2019, likely because of decreased relapse rates over time as NRM and short-term survival remained stable.
Keyword(s): Acute lymphoblastic leukemia, Allogeneic hematopoietic stem cell transplant, Survival
Abstract: EP359
Type: E-Poster Presentation
Session title: Acute lymphoblastic leukemia - Clinical
Background
Survival after allogeneic hematopoietic cell transplantation (HCT) of high-risk acute lymphoblastic leukemia (ALL) is challenged by high risk of relapse and non-relapse mortality (NRM) due to conditioning toxicity or graft-versus-host disease (GvHD).
Aims
We aimed to investigate temporal trends of survival in a nationwide population-based cohort study of adults (≥18 years) who received HCT for ALL in Denmark between 2000–2019.
Methods
Indications for HCT comprised high-risk ALL (including Philadelphia chromosome positive [Ph+] ALL) or ALL in >1st complete remission (CR). From 2011, non-myeloablative HCT was perfomed for patients >50 years or with comorbidities, and from 2012, Ph+ patients received a tyrosine kinase inhibitor one year post-HCT. Temporal trends in overall survival (OS) were examined in a Royston–Parmar survival model. A non-mixture cure model was used to estimate temporal trends in short- and long-term survival, respectively (long-term survival estimated as the cure fraction, i.e. the fraction of patients who experienced no excess mortality compared to the Danish general population matched on calendar year, age and sex). Hazard ratios (HR) of relapse and NRM were estimated in cause-specific Cox models. Cumulative incidences of HCT outcomes were calculated by the Aalen-Johansen method and compared between patients transplanted in the earliest vs. latest quartile (years 2000–2005 vs. 2016–2019).
Results
From 2000 to 2019, 181 adults were transplanted for ALL in Denmark; 83% with B-cell, 17% with T-cell and 31% with Ph+ ALL. Median (min–max) age at transplant was 36 (18–74) years. Most patients (72%) were transplanted in CR1, and the median time from diagnosis to transplant was 7 months. The most common regimen was myeloablative (84%) transplant (Eto- or CyTBI) with a matched unrelated donor (56%). In later time periods, more patients were transplanted in CR1 and with non-myeloablative conditioning, while the proportion of patients with Ph+ ALL was constant. At a median follow-up of 8.1 years, 77 (43%) patients had died. The 2- and 5-year Kaplan–Meier OS (95% CI) were 69% (63%, 76%) and 62% (55%, 70%) in the entire cohort. OS increased with year of HCT (p = 0.03) with an estimated 2-year OS (95% CI) of 49% (27%, 66%) in patients transplanted in year 2000 vs. 77% (59%, 88%) in 2019 (Figure). The estimated cure fraction increased over time (odds ratio for cure per calendar year increase: 1.08; 95% CI: 1.01, 1.15; p = 0.03), whereas the short-term excess hazard of dying did not change significantly (HR per calendar year: 1.00; 95% CI: 0.93, 1.07; p = 0.97). This was reflected in the decreased risk of relapse over time (HR 0.92 per calendar year; 95% CI: 0.87, 0.98, p = 0.01; 2-year cumulative incidence in years 2000–2005: 26% [95% CI: 12%, 39%] vs. 12% [95% CI: 3%, 21%] in years 2016–2019), and the stable risk of NRM (HR 0.98 per calendar year; 95% CI: 0.93, 1.04, p = 0.49; 2-year cumulative incidence in years 2000–2005: 21% [95% CI: 9%, 33%] vs. 16% [95% CI: 6%, 26%] in years 2016–2019). The incidence of GvHD did not change markedly over time (grade II–IV acute GvHD: 35% [95% CI: 20%, 49%] in years 2000–2005 vs. 37% [95% CI: 24%, 51%] in years 2016–2019; chronic GvHD at 2 years: 40% [95% CI: 25%, 54%] in years 2000–2005 vs. 51% [95% CI: 37%, 65%] in years 2016–2019).
Conclusion
In a nationwide cohort study of HCT-treated ALL-patients, we found an improved long-term survival from 2000 to 2019, likely because of decreased relapse rates over time as NRM and short-term survival remained stable.
Keyword(s): Acute lymphoblastic leukemia, Allogeneic hematopoietic stem cell transplant, Survival


