
Contributions
Abstract: EP350
Type: E-Poster Presentation
Session title: Acute lymphoblastic leukemia - Clinical
Background
SARS-CoV-2 infection has bimodal distribution in Europe with a 1st wave in March-June 2020 and a 2nd in September 2020-February 2021. In cancer patients (pts) the lethality of COVID-19 infection was 25%>35% in the 1st wave. Comparison on impact of COVID-19 infection in the 1st vs. 2nd waves have not been performed in ALL.
Aims
We compared the frequency, clinical characteristics and outcome of adults with ALL and COVID-19 infection in the 1st vs. 2nd waves in Spain.
Methods
Between March 1, 2020-May 31, 2020, and between September 12, 2020- January 12, 2021 (date of vaccination onset in Spain), a registry from the PETHEMA (Programa Español de Tratamientos en Hematologia) and GETH (Grupo Español de Trasplante Hematopoyético y Terapia Celular) groups prospectively recruited adult ALL pts with COVID-19 infection confirmed by PCR. Demographic and clinical characteristics of ALL and COVID-19 infection, comorbidities, treatment and outcome were collected and compared in the two periods. In addition, prognostic factors for survival were analyzed.
Results
Fifty-six patients were collected in 82 centers contacted, 4 of them being excluded (COVID infection >3 yr. after end of ALL therapy [n=3] and Burkitt lymphoma [n=1]). Twenty-eight pts were collected in the 1st wave and 24 in the 2nd. Median age was 46 (range 20-83), (34 pts [65%] >40 yr). Comorbidities were present in 18 pts (35%). ALL was of B-cell precursors in 38 pts (74%) (Ph+ in 8, 15%). Thirty-one pts (60%) were under frontline treatment, 16 (31%) in rescue, 1 (2%) palliative and 4 (7%) had recently finished the therapy. Eight pts had received allogeneic HSCT (5 of them at COVID-19 infection diagnosis), CAR T (n=1, 2 yr prior to COVID-19 infection) or received immunotherapy (inotuzumab, n=6, 2 at COVID-19 infection, and blinatumomab, n=1, prior to COVID-19 infection). Eleven pts were receiving immunosuppressive drugs at COVID infection (fludarabine in 6, among others).
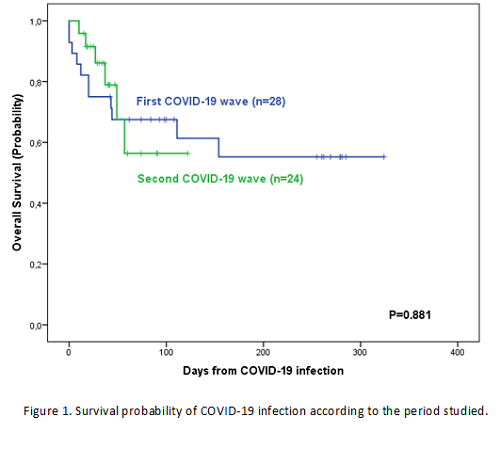
No significant differences were observed in ALL characteristics in the two COVID-19 waves, except for a significantly higher number of patients on first line therapy in the second wave, and a higher frequency of severe neutropenia and lymphocytopenia in the first wave. COVID19 therapy was different in the two periods, with significantly higher use of hydroxychloroquine, remdesivir and lopinavir-ritonavir in the first wave and corticosteroids in the second wave. No significant differences were observed in need of oxygen support (12 vs. 8 pts), ICU requirement (7 vs. 4 pts), days in ICU (medians 16 vs. 21) and time to COVID infection recovery (medians 17 vs. 13 days). Seventeen patients (33%) died (11 vs. 6), being death attributed to COVID infection in 15 (29%), without significant differences in the 100-day survival probabilities (Figure 1). By multivariable analysis only comorbidities at COVID-19 infection had a negative impact on survival (HR: 5.358 [95% CI: 1.875; 15.313]).
Conclusion
COVID-19 infection was frequent in ALL pts, especially in those with advanced age and under ALL frontline or rescue therapy. The frequency of severe COVID-19 infection and mortality were high, with negative impact of comorbidities on survival. No significant differences were observed in ALL characteristics, response to therapy and outcome in the two waves of COVID infection. The poor outcome of COVID infection makes vaccination a priority for ALL patients in this pandemic period.
Supported in part by 2017 SGR288 (GRC) Generalitat de Catalunya and “la Caixa” Foundation.
Keyword(s): Acute lymphoblastic leukemia, COVID-19, Prognosis
Abstract: EP350
Type: E-Poster Presentation
Session title: Acute lymphoblastic leukemia - Clinical
Background
SARS-CoV-2 infection has bimodal distribution in Europe with a 1st wave in March-June 2020 and a 2nd in September 2020-February 2021. In cancer patients (pts) the lethality of COVID-19 infection was 25%>35% in the 1st wave. Comparison on impact of COVID-19 infection in the 1st vs. 2nd waves have not been performed in ALL.
Aims
We compared the frequency, clinical characteristics and outcome of adults with ALL and COVID-19 infection in the 1st vs. 2nd waves in Spain.
Methods
Between March 1, 2020-May 31, 2020, and between September 12, 2020- January 12, 2021 (date of vaccination onset in Spain), a registry from the PETHEMA (Programa Español de Tratamientos en Hematologia) and GETH (Grupo Español de Trasplante Hematopoyético y Terapia Celular) groups prospectively recruited adult ALL pts with COVID-19 infection confirmed by PCR. Demographic and clinical characteristics of ALL and COVID-19 infection, comorbidities, treatment and outcome were collected and compared in the two periods. In addition, prognostic factors for survival were analyzed.
Results
Fifty-six patients were collected in 82 centers contacted, 4 of them being excluded (COVID infection >3 yr. after end of ALL therapy [n=3] and Burkitt lymphoma [n=1]). Twenty-eight pts were collected in the 1st wave and 24 in the 2nd. Median age was 46 (range 20-83), (34 pts [65%] >40 yr). Comorbidities were present in 18 pts (35%). ALL was of B-cell precursors in 38 pts (74%) (Ph+ in 8, 15%). Thirty-one pts (60%) were under frontline treatment, 16 (31%) in rescue, 1 (2%) palliative and 4 (7%) had recently finished the therapy. Eight pts had received allogeneic HSCT (5 of them at COVID-19 infection diagnosis), CAR T (n=1, 2 yr prior to COVID-19 infection) or received immunotherapy (inotuzumab, n=6, 2 at COVID-19 infection, and blinatumomab, n=1, prior to COVID-19 infection). Eleven pts were receiving immunosuppressive drugs at COVID infection (fludarabine in 6, among others).
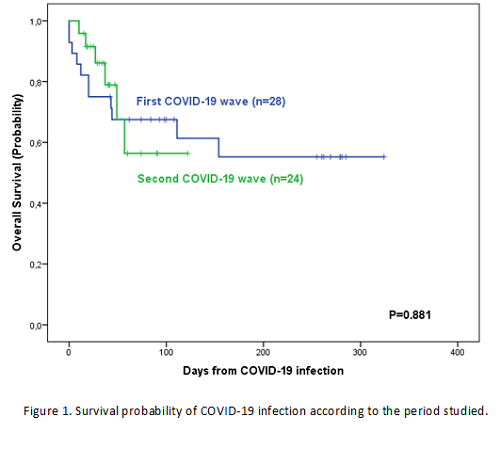
No significant differences were observed in ALL characteristics in the two COVID-19 waves, except for a significantly higher number of patients on first line therapy in the second wave, and a higher frequency of severe neutropenia and lymphocytopenia in the first wave. COVID19 therapy was different in the two periods, with significantly higher use of hydroxychloroquine, remdesivir and lopinavir-ritonavir in the first wave and corticosteroids in the second wave. No significant differences were observed in need of oxygen support (12 vs. 8 pts), ICU requirement (7 vs. 4 pts), days in ICU (medians 16 vs. 21) and time to COVID infection recovery (medians 17 vs. 13 days). Seventeen patients (33%) died (11 vs. 6), being death attributed to COVID infection in 15 (29%), without significant differences in the 100-day survival probabilities (Figure 1). By multivariable analysis only comorbidities at COVID-19 infection had a negative impact on survival (HR: 5.358 [95% CI: 1.875; 15.313]).
Conclusion
COVID-19 infection was frequent in ALL pts, especially in those with advanced age and under ALL frontline or rescue therapy. The frequency of severe COVID-19 infection and mortality were high, with negative impact of comorbidities on survival. No significant differences were observed in ALL characteristics, response to therapy and outcome in the two waves of COVID infection. The poor outcome of COVID infection makes vaccination a priority for ALL patients in this pandemic period.
Supported in part by 2017 SGR288 (GRC) Generalitat de Catalunya and “la Caixa” Foundation.
Keyword(s): Acute lymphoblastic leukemia, COVID-19, Prognosis


