
Contributions
Abstract: EP1345
Type: E-Poster Presentation
Session title: Transfusion medicine
Background
According to the literature, up to 20% of platelet transfusions are considered inadequate, increasing platelet consumption and exposure to patients at risk.
Aims
The objective of this study is to know the incidence of inadequate platelet transfusion in our center and to determine areas of improvement.
Methods
Platelet transfusions performed in November 2020 at our center were reviewed retrospectively. Each transfusion was considered independently. Intra-operating room requests were excluded. Criteria of appropriate platelet transfusion set in the Guide on the Transfusion of Blood Components and Plasma Derivatives of the Spanish Society of Blood Transfusion and Cell Therapy (5th ed) were used: stable patients with central thrombocytopenia and platelet <10x109/L, platelets <20x109/L in non-stable patients (> 38 Celsius degrees fever, signs of ≥ WHO grade 2 haemorrhage), platelets < 50x109/L in patients who will undergo major surgical and/or invasive procedures or have signs of ≥ WHO grade 3 bleeding and platelets is < 80x109/L in case of central nervous system or eye involvement.
Results
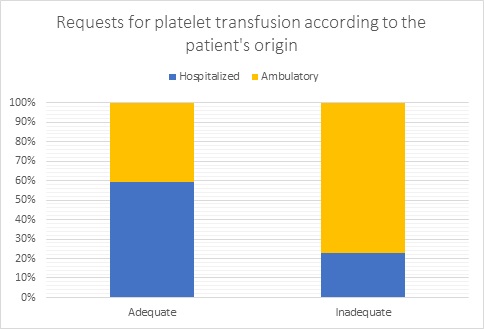
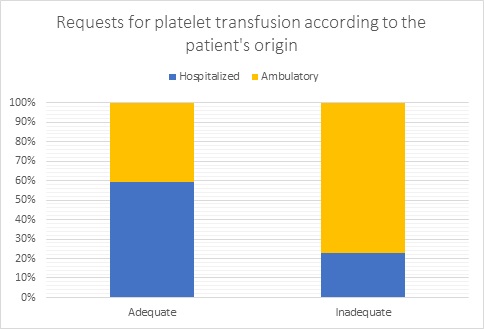
Our center is a tertiary University Hospital with a large Stem Cell Transplantation program and important cardiac surgery department. 335 transfusion episodes were reviewed in 86 patients with mean age of 55 years (0-90). It involved 476 units of platelets. 49.4% were women (165/335), 78.5% (263/335) were indicated by the Hematology service and 11.4% (38/335) because of surgical procedures. 283 transfusions (84.4%) were performed in hospitalized patients compared to 52 (15.5%) outpatients. In 5 patients (5.8%) tranexamic acid was associated. 86% (288/335) of platelet transfusions were correctly indicated while 14% (47/335) did not meet the criteria described above, 29 patients (33%) were inadequately transfused with 49 platelet units (10,6% of total). No significant differences were found with respect to the requesting service. The main indication of platelet transfusion was stable thrombocytopenias with platelet values between 10x109/L and 20x109/L and it is this indication that has the highest frequency of inadequate transfusion. A significant difference was observed in the percentage of units suitable indications in outpatients versus admitted (40% vs 12%, p <0.005).
Conclusion
There is a high percentage of inadequate platelet transfusions, similar to the incidence referred in the literature. The main area of improvement is transfusion in outpatients. The development of training programmes and prescription aid systems can help to improve these outcomes.
Keyword(s): Hemorrhage, Platelet, Thrombocytopenia, Transfusion
Abstract: EP1345
Type: E-Poster Presentation
Session title: Transfusion medicine
Background
According to the literature, up to 20% of platelet transfusions are considered inadequate, increasing platelet consumption and exposure to patients at risk.
Aims
The objective of this study is to know the incidence of inadequate platelet transfusion in our center and to determine areas of improvement.
Methods
Platelet transfusions performed in November 2020 at our center were reviewed retrospectively. Each transfusion was considered independently. Intra-operating room requests were excluded. Criteria of appropriate platelet transfusion set in the Guide on the Transfusion of Blood Components and Plasma Derivatives of the Spanish Society of Blood Transfusion and Cell Therapy (5th ed) were used: stable patients with central thrombocytopenia and platelet <10x109/L, platelets <20x109/L in non-stable patients (> 38 Celsius degrees fever, signs of ≥ WHO grade 2 haemorrhage), platelets < 50x109/L in patients who will undergo major surgical and/or invasive procedures or have signs of ≥ WHO grade 3 bleeding and platelets is < 80x109/L in case of central nervous system or eye involvement.
Results
Our center is a tertiary University Hospital with a large Stem Cell Transplantation program and important cardiac surgery department. 335 transfusion episodes were reviewed in 86 patients with mean age of 55 years (0-90). It involved 476 units of platelets. 49.4% were women (165/335), 78.5% (263/335) were indicated by the Hematology service and 11.4% (38/335) because of surgical procedures. 283 transfusions (84.4%) were performed in hospitalized patients compared to 52 (15.5%) outpatients. In 5 patients (5.8%) tranexamic acid was associated. 86% (288/335) of platelet transfusions were correctly indicated while 14% (47/335) did not meet the criteria described above, 29 patients (33%) were inadequately transfused with 49 platelet units (10,6% of total). No significant differences were found with respect to the requesting service. The main indication of platelet transfusion was stable thrombocytopenias with platelet values between 10x109/L and 20x109/L and it is this indication that has the highest frequency of inadequate transfusion. A significant difference was observed in the percentage of units suitable indications in outpatients versus admitted (40% vs 12%, p <0.005).
Conclusion
There is a high percentage of inadequate platelet transfusions, similar to the incidence referred in the literature. The main area of improvement is transfusion in outpatients. The development of training programmes and prescription aid systems can help to improve these outcomes.
Keyword(s): Hemorrhage, Platelet, Thrombocytopenia, Transfusion


