
Contributions
Abstract: EP1328
Type: E-Poster Presentation
Session title: Thrombosis and vascular biology - Biology & Translational Research
Background
Platelet adhesion is an important process in primary haemostasis and thrombus formation. Von Willebrand factor (VWF) is a key mediator of platelet adhesion at sites of vascular injury under high shear rates. Recent studies showed that VWF becomes highly reactive with platelets and leukocytes upon unfolding into a stretched conformation, at shear rates above the critical value, which occur at sites of arterial stenosis and injury. Activated VWF and platelets, adhered to injured vessel wall, may serve as sites of leukocyte recruitment under flow conditions and predispose to the propagation of inflammation and thrombosis.
Aims
The aim of the study was to investigate platelet adhesion and leukocyte recruitment in whole blood under high shear rates.
Methods
Venous blood from 7 healthy volunteers was collected from the cubital vein into PPACK solution at final concentration of 100 µM or into EDTA (1.6 mg/ml). To study the kinetics of cell adhesion to collagen we developed a laser optical system that utilizes special optical and microfluidic techniques. The microfluidic optical system consists of a cell assembly with a disposable flow chamber, a specialised optical prism system with a semiconductor laser and a photodetector. Shear stress-induced adhesion of blood cells to type I collagen-coated surface of a perfusion chamber was registered during 15 minutes of circulation of whole blood samples at shear rate of 2300 s-1. After 15 minutes of perfusion flow chambers were fixed with 1% formalin solution, stained by Giemsa staining and 4′,6-diamidino-2-phenylindole (DAPI). Platelet GP Ib and GP IIb/IIIa receptors were blocked using monoclonal antibodies.
Results
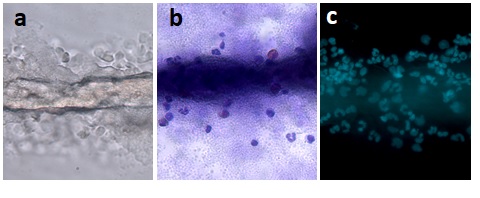
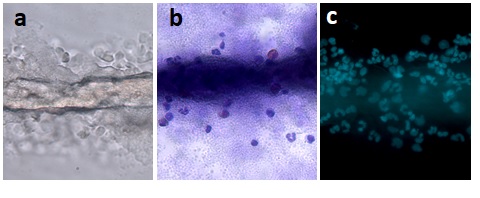
Cell adhesion was quantified by measuring the intensity of scattered light after 15 min of perfusion and was 0.35±0.10 V in control samples, 0.25±0.08 V in samples after addition of anti-GP Ib and 0.07±0.03 V after addition of anti-GP IIb/IIIa antibodies (p=0.002). In blood samples with EDTA the intensity of scattered light was 0.06±0.02. Microscopy of perfusion chambers revealed large protein structures in the form of long strands. They were attached to a collagen surface and stretched along the streamline (Fig. 1a). Microscopy of perfusion chambers after Giemsa staining revealed that the protein structures were co-localized with leukocytes and platelets (Fig. 1b). Fluorescence microscopy of samples after staining with DAPI confirmed that there are leukocytes in this structure (fig. 1c).
Figure 1. Platelet adhesion and leukocyte recruitment to a collagen-coated surface at shear rate of 2300 s-1. (a) Transmitted optical microscopy; (b) Microscopy with Giemsa staining; (d) staining with 4′,6-diamidino-2-phenylindole (DAPI).
Conclusion
Our data demonstrate that platelet adhesion and leukocyte recruitment to collagen coated surface at high shear rates is mediated by the complex interaction of von Willebrand factor and platelet GP receptors.
Keyword(s): Leukocytes, Platelet, Shear stress, Von Willebrand factor (vWF)
Abstract: EP1328
Type: E-Poster Presentation
Session title: Thrombosis and vascular biology - Biology & Translational Research
Background
Platelet adhesion is an important process in primary haemostasis and thrombus formation. Von Willebrand factor (VWF) is a key mediator of platelet adhesion at sites of vascular injury under high shear rates. Recent studies showed that VWF becomes highly reactive with platelets and leukocytes upon unfolding into a stretched conformation, at shear rates above the critical value, which occur at sites of arterial stenosis and injury. Activated VWF and platelets, adhered to injured vessel wall, may serve as sites of leukocyte recruitment under flow conditions and predispose to the propagation of inflammation and thrombosis.
Aims
The aim of the study was to investigate platelet adhesion and leukocyte recruitment in whole blood under high shear rates.
Methods
Venous blood from 7 healthy volunteers was collected from the cubital vein into PPACK solution at final concentration of 100 µM or into EDTA (1.6 mg/ml). To study the kinetics of cell adhesion to collagen we developed a laser optical system that utilizes special optical and microfluidic techniques. The microfluidic optical system consists of a cell assembly with a disposable flow chamber, a specialised optical prism system with a semiconductor laser and a photodetector. Shear stress-induced adhesion of blood cells to type I collagen-coated surface of a perfusion chamber was registered during 15 minutes of circulation of whole blood samples at shear rate of 2300 s-1. After 15 minutes of perfusion flow chambers were fixed with 1% formalin solution, stained by Giemsa staining and 4′,6-diamidino-2-phenylindole (DAPI). Platelet GP Ib and GP IIb/IIIa receptors were blocked using monoclonal antibodies.
Results
Cell adhesion was quantified by measuring the intensity of scattered light after 15 min of perfusion and was 0.35±0.10 V in control samples, 0.25±0.08 V in samples after addition of anti-GP Ib and 0.07±0.03 V after addition of anti-GP IIb/IIIa antibodies (p=0.002). In blood samples with EDTA the intensity of scattered light was 0.06±0.02. Microscopy of perfusion chambers revealed large protein structures in the form of long strands. They were attached to a collagen surface and stretched along the streamline (Fig. 1a). Microscopy of perfusion chambers after Giemsa staining revealed that the protein structures were co-localized with leukocytes and platelets (Fig. 1b). Fluorescence microscopy of samples after staining with DAPI confirmed that there are leukocytes in this structure (fig. 1c).
Figure 1. Platelet adhesion and leukocyte recruitment to a collagen-coated surface at shear rate of 2300 s-1. (a) Transmitted optical microscopy; (b) Microscopy with Giemsa staining; (d) staining with 4′,6-diamidino-2-phenylindole (DAPI).
Conclusion
Our data demonstrate that platelet adhesion and leukocyte recruitment to collagen coated surface at high shear rates is mediated by the complex interaction of von Willebrand factor and platelet GP receptors.
Keyword(s): Leukocytes, Platelet, Shear stress, Von Willebrand factor (vWF)


