
Contributions
Abstract: EP1303
Type: E-Poster Presentation
Session title: Thalassemias
Background
Secondary graft failure (SGF) is a major obstacle in allogeneic hematopoietic stem cell transplantation for patients with thalassemia major(TM). However, the impact of the persisting mixed chimerism (MC) on transplant outcome remains controversial.
Aims
To assess risk factors of mixed chimerism and to evaluate possible correlations between mixed chimerism and transplantation outcomes.
Methods
A total of 618 patients with thalassemia major (TM) underwent allogeneic HSCT from December2008 until December 2019 were identified with median age of 6 years old (1-23) and median follow up time of 70 months(1-135), from HLA-identical sibling donors (SD) (n=212; 34.3%), unrelated donors (UD, n=313; 50.6%),sibling Cord blood(CB, n=49,7.9%)and parent donors (PD, n=44,7.1%). Source of graft were 538 (87.1%) from peripheral stem cells, 32(5.2%) from bone marrow and 48(7.8%)from sibling cord blood. Cy+Bu+Flu+TT+ATG conditioning regimen was used in 416 pts while a reduced conditioning regimen Cy+Bu+Flu+ATG was used for 167pts and Cy+Bu+Flu for the other 35 pts.
Results
Overall Survival (OS), Thalassemia-Free survival (TFS), Transplantation-related mortality (TRM) and graft rejection (GR) for the entire group were 94.8%, 92.7%,5.2% and 2.4% respectively.MC was presented in 70 pts, with median present time 4 months (1-59 months). The cumulative incidence MC was 12.4% .
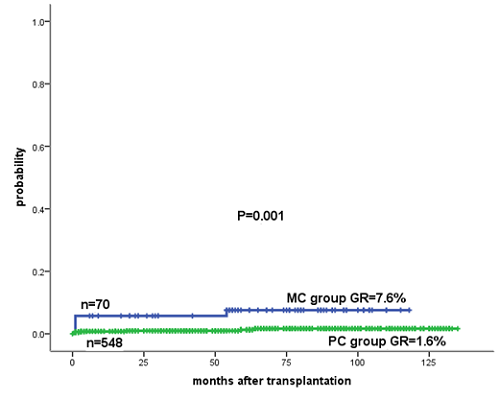
No significant difference was observed in OS and Thalassemia-Free survival (TFS) between MC and full donor chimerism (FC) pts. The cumulative probability of OS, TFS between MC pts and FC pts was 97.1% vs. 94.4% (P=0.343) and 89.6% vs. 93.2% (P=0.272),respectively. However, the incidence of MC was significantly associated with the development of graft failure/rejection. Graft failure occurred in 5 pts in the MC group vs.7 pts in the FC group, the corresponding incidence were 7.6% vs. 1.6 % respectively. (P =0.001, Figure ).
Acute GVHD incidence was much lower in MC pts than in FC pts (2.9% vs. 12.7%, P=0.022, ), whereas MC pts had significantly higher chronic GVHD(16.8% vs. 4.2%, P=0.000 ).MC was associated with an increased risk of chronic GVHD, mostly were DLI derived
Patients receiving stem cells from cord blood of matched sibling donors had a high risk of MC.MC incidence of stem cell source from peripheral blood(PB), bone marrow(BM), cord blood (CB)were 10.6%, 10%, 34.2% respectively.(P=0.000).Unrelated donors had a lower risk of MC than sibling donors. Incidence of MC from unrelated donors was 9.5% vs. 16.1% from sibling donors (P=0.007).
Intravenous Thiotepa (TT) in combination with Busulfan (Bu), cyclophosphamide (Cy) anti-thymocyte globulin (ATG ) on HSCT could reduce the risk of MC. The corresponding incidence of MC in Cy+Bu+Flu+TT+ATG, Cy+Bu+Flu+ATG, Cy+Bu+Flu conditioning regimen were 9.2%,15.9%,40.9% resepectively(P=0.000).
There was also a significant difference in chimerism based on donor-recipient gender pairing (P = 0.041): male grafts into male patients having the greatest risk of MC and female grafts into female patients having the least. Patients who under 9 years old had a higher risk of MC than that of pts>9 years old (P=0.018).
Conclusion
Our results show that patients who presented mixed chimerism showed a similar post-transplant outcome in OS and TFS but was associated with higher risk of graft failue.Patients receiving stem cells from CB had a high risk of MC than from PBSC. Reduced nonmyeloablative approach capable of achieving allogeneic mixed hematopoietic chimerism. Our data suggests that Cy+Bu+Flu+TT+ATG is a preferred conditioning regimenfor TM patients could reduce the risk of mixed chimerism.
Keyword(s): HSCT, Mixed chimerism, Risk factor, Thalassemia
Abstract: EP1303
Type: E-Poster Presentation
Session title: Thalassemias
Background
Secondary graft failure (SGF) is a major obstacle in allogeneic hematopoietic stem cell transplantation for patients with thalassemia major(TM). However, the impact of the persisting mixed chimerism (MC) on transplant outcome remains controversial.
Aims
To assess risk factors of mixed chimerism and to evaluate possible correlations between mixed chimerism and transplantation outcomes.
Methods
A total of 618 patients with thalassemia major (TM) underwent allogeneic HSCT from December2008 until December 2019 were identified with median age of 6 years old (1-23) and median follow up time of 70 months(1-135), from HLA-identical sibling donors (SD) (n=212; 34.3%), unrelated donors (UD, n=313; 50.6%),sibling Cord blood(CB, n=49,7.9%)and parent donors (PD, n=44,7.1%). Source of graft were 538 (87.1%) from peripheral stem cells, 32(5.2%) from bone marrow and 48(7.8%)from sibling cord blood. Cy+Bu+Flu+TT+ATG conditioning regimen was used in 416 pts while a reduced conditioning regimen Cy+Bu+Flu+ATG was used for 167pts and Cy+Bu+Flu for the other 35 pts.
Results
Overall Survival (OS), Thalassemia-Free survival (TFS), Transplantation-related mortality (TRM) and graft rejection (GR) for the entire group were 94.8%, 92.7%,5.2% and 2.4% respectively.MC was presented in 70 pts, with median present time 4 months (1-59 months). The cumulative incidence MC was 12.4% .
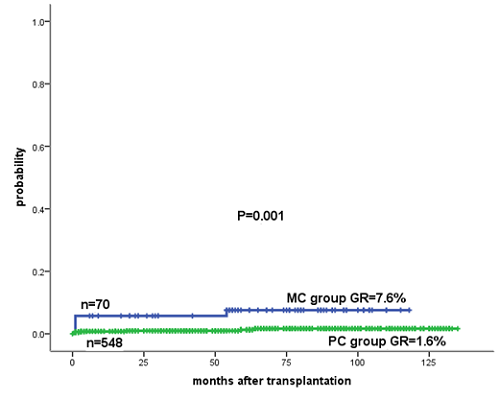
No significant difference was observed in OS and Thalassemia-Free survival (TFS) between MC and full donor chimerism (FC) pts. The cumulative probability of OS, TFS between MC pts and FC pts was 97.1% vs. 94.4% (P=0.343) and 89.6% vs. 93.2% (P=0.272),respectively. However, the incidence of MC was significantly associated with the development of graft failure/rejection. Graft failure occurred in 5 pts in the MC group vs.7 pts in the FC group, the corresponding incidence were 7.6% vs. 1.6 % respectively. (P =0.001, Figure ).
Acute GVHD incidence was much lower in MC pts than in FC pts (2.9% vs. 12.7%, P=0.022, ), whereas MC pts had significantly higher chronic GVHD(16.8% vs. 4.2%, P=0.000 ).MC was associated with an increased risk of chronic GVHD, mostly were DLI derived
Patients receiving stem cells from cord blood of matched sibling donors had a high risk of MC.MC incidence of stem cell source from peripheral blood(PB), bone marrow(BM), cord blood (CB)were 10.6%, 10%, 34.2% respectively.(P=0.000).Unrelated donors had a lower risk of MC than sibling donors. Incidence of MC from unrelated donors was 9.5% vs. 16.1% from sibling donors (P=0.007).
Intravenous Thiotepa (TT) in combination with Busulfan (Bu), cyclophosphamide (Cy) anti-thymocyte globulin (ATG ) on HSCT could reduce the risk of MC. The corresponding incidence of MC in Cy+Bu+Flu+TT+ATG, Cy+Bu+Flu+ATG, Cy+Bu+Flu conditioning regimen were 9.2%,15.9%,40.9% resepectively(P=0.000).
There was also a significant difference in chimerism based on donor-recipient gender pairing (P = 0.041): male grafts into male patients having the greatest risk of MC and female grafts into female patients having the least. Patients who under 9 years old had a higher risk of MC than that of pts>9 years old (P=0.018).
Conclusion
Our results show that patients who presented mixed chimerism showed a similar post-transplant outcome in OS and TFS but was associated with higher risk of graft failue.Patients receiving stem cells from CB had a high risk of MC than from PBSC. Reduced nonmyeloablative approach capable of achieving allogeneic mixed hematopoietic chimerism. Our data suggests that Cy+Bu+Flu+TT+ATG is a preferred conditioning regimenfor TM patients could reduce the risk of mixed chimerism.
Keyword(s): HSCT, Mixed chimerism, Risk factor, Thalassemia


