
Contributions
Abstract: EP1291
Type: E-Poster Presentation
Session title: Stem cell transplantation - Clinical
Background
Sex differences play a relevant role in cancer susceptibility, incidence and survival, with male patients being at higher risk. Genetic, epigenetic and hormonal factors are involved in such differences, and a better understanding of their close interplay in the mechanisms of cancer could improve its prevention and therapy. However, assessing the actual weight of each one of these factors is challenging.
Aims
This study aims to explore sex differences in first and advanced-line therapy outcomes in pediatric oncology. In particular, we investigated whether the known sex differences occurring after first-line therapy, and leading to a higher number of male patients requiring Hematopoietic Stem Cells Trasplantation (HSCT), persist after transplant.This study setting may represent an experimental human model that reveals the possible effects of the impairment of gonadal hormones on cancer progression, which is poorly explored in the literature.
Methods
The study is a Single-center retrospective cohort observational study. Population of the study are pediatric patients between 0 and 18 years of age admitted for hematological malignances between 2000 and 2018 who underwent allogeneic or autologous HSCT at the pediatric Department of Oncology of the Institute for Maternal and Child Health of Trieste. As part of the HSCT course, participants underwent a conditioning regimen either with high-dose (myeloablative) chemotherapy or with total body irradiation (TBI), both of which exert a substantial impairment on gonadal function.
Results
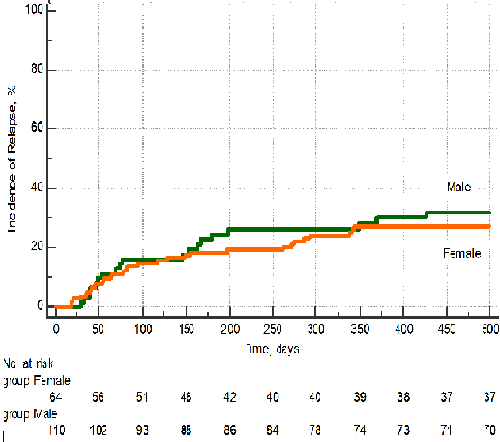
Out of a total of 485 patients (280 males, 205 females) admitted for malignant diseases between 2000 and 2018, 174 patients (111 males and 63 females) had a high-risk form of acute lymphatic leukemia, acute myeloid leukemia, myelodysplasia or solid tumors requiring HSCT. Among these patients 15 males (9%) and 6 females (3%) died from primary disease relapse, providing a DRM of 12%. Fourteen males (8%) and 13 females (7%) died from transplant-related causes, providing a TRM of 15%. No statistically significant differences between males and females were found in terms of DRM and TRM (P > .05). The OS was 72%, including 82 male and 44 females. One hundred eleven patients (64%) showed a disease-free survival (DFS), including 72 males and 39 females. The Cumulative Relapse Incidence (CRI) was 21%, with 25 males and 11 females having a primary disease relapse. In addition, we analyzed differences in OS, EFS, early death, TRM, DRM, and the need for a further HSCT by comparing donor-recipient pairs matched and mismatched for sex and by comparing two age groups (<12 years, >12 years). No statistically significant differences for HSCT-related complications (mucositis, gastrointestinal, hepatic, lung and kidney toxicity, and GvHD) were found between donor-recipient pairs matched and mismatched for sex. (P > .05) Similarly, no statistically significant differences in HSCT complications were found between males and females when comparing two age groups (<12 years, >12 years)
Conclusion
While the number of males needing HSCT was almost double that of females, confirming the well-known “male disadvantage” with respect to cancer reported in the literature, no sex-related differences in terms of overall survival, cancer relapse, or complications were reported after HSCT exposure. These findings suggest that the existing sex differences in cancer risk ab initio can be modified by HSCT and its preliminary conditioning regimen, implicating a role of hormonal factors in cancer mechanisms and management.
Keyword(s): Gender, HSCT
Abstract: EP1291
Type: E-Poster Presentation
Session title: Stem cell transplantation - Clinical
Background
Sex differences play a relevant role in cancer susceptibility, incidence and survival, with male patients being at higher risk. Genetic, epigenetic and hormonal factors are involved in such differences, and a better understanding of their close interplay in the mechanisms of cancer could improve its prevention and therapy. However, assessing the actual weight of each one of these factors is challenging.
Aims
This study aims to explore sex differences in first and advanced-line therapy outcomes in pediatric oncology. In particular, we investigated whether the known sex differences occurring after first-line therapy, and leading to a higher number of male patients requiring Hematopoietic Stem Cells Trasplantation (HSCT), persist after transplant.This study setting may represent an experimental human model that reveals the possible effects of the impairment of gonadal hormones on cancer progression, which is poorly explored in the literature.
Methods
The study is a Single-center retrospective cohort observational study. Population of the study are pediatric patients between 0 and 18 years of age admitted for hematological malignances between 2000 and 2018 who underwent allogeneic or autologous HSCT at the pediatric Department of Oncology of the Institute for Maternal and Child Health of Trieste. As part of the HSCT course, participants underwent a conditioning regimen either with high-dose (myeloablative) chemotherapy or with total body irradiation (TBI), both of which exert a substantial impairment on gonadal function.
Results
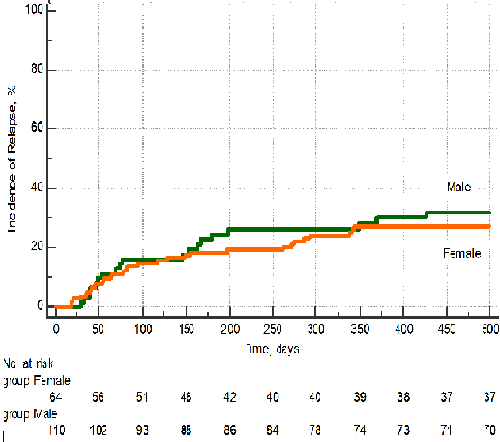
Out of a total of 485 patients (280 males, 205 females) admitted for malignant diseases between 2000 and 2018, 174 patients (111 males and 63 females) had a high-risk form of acute lymphatic leukemia, acute myeloid leukemia, myelodysplasia or solid tumors requiring HSCT. Among these patients 15 males (9%) and 6 females (3%) died from primary disease relapse, providing a DRM of 12%. Fourteen males (8%) and 13 females (7%) died from transplant-related causes, providing a TRM of 15%. No statistically significant differences between males and females were found in terms of DRM and TRM (P > .05). The OS was 72%, including 82 male and 44 females. One hundred eleven patients (64%) showed a disease-free survival (DFS), including 72 males and 39 females. The Cumulative Relapse Incidence (CRI) was 21%, with 25 males and 11 females having a primary disease relapse. In addition, we analyzed differences in OS, EFS, early death, TRM, DRM, and the need for a further HSCT by comparing donor-recipient pairs matched and mismatched for sex and by comparing two age groups (<12 years, >12 years). No statistically significant differences for HSCT-related complications (mucositis, gastrointestinal, hepatic, lung and kidney toxicity, and GvHD) were found between donor-recipient pairs matched and mismatched for sex. (P > .05) Similarly, no statistically significant differences in HSCT complications were found between males and females when comparing two age groups (<12 years, >12 years)
Conclusion
While the number of males needing HSCT was almost double that of females, confirming the well-known “male disadvantage” with respect to cancer reported in the literature, no sex-related differences in terms of overall survival, cancer relapse, or complications were reported after HSCT exposure. These findings suggest that the existing sex differences in cancer risk ab initio can be modified by HSCT and its preliminary conditioning regimen, implicating a role of hormonal factors in cancer mechanisms and management.
Keyword(s): Gender, HSCT


