
Contributions
Abstract: EP1279
Type: E-Poster Presentation
Session title: Stem cell transplantation - Clinical
Background
The expected median survival of intermediate risk and high-risk myelofibrosis (MF) defined by dynamic international prognostic staging system (DIPSS) is of 2.9 and 1.3 years, respectively.
For that reason, allogeneic hematopoietic stem cell transplant (HSCT) is still considered the only curative option for those patients that are eligible for it.
The use of peripheral blood stem cell (PBSC) as graft source is allowing a fast engraftment, but there is still uncertainty among different centres about the most appropriate conditioning regimen in MF and the maximum age limit for myeloablative (MA) conditioning.
Aims
Herein we report the outcome of myeloablative HSCT in patients older than55 with high-risk MF as defined by DIPSS.
Methods
Between April 2012 and December 2018, 22 patients (10 high risk, 12 intermediate-2) with a median age of 61 (range 44-68 years) had full matched allogeneic stem cell transplant. HSCT was performed with GCSF mobilised PBSC. Conditioning protocol was with fludarabine 15 mg/m2 days -9, -8, -7, -6, -5, busulfan 3.2 mg/Kg days -6, -5, -4, -3; graft versus host disease (GVHD) prophylaxis consisted of thymoglobulin before transplant (ATG 5.5 mg/Kg until January 2015; ATG 5 mg/Kg since March 2016) and single agent ciclosporin 1.5 mg/Kg (therapeutic level of 200) until d+90 and then tapered. A median of 5x106 CD34+/Kg was infused (3.2 – 6). Donors were: 10 siblings, 11 unrelated donor, 1 mismatched unrelated donor.
Results
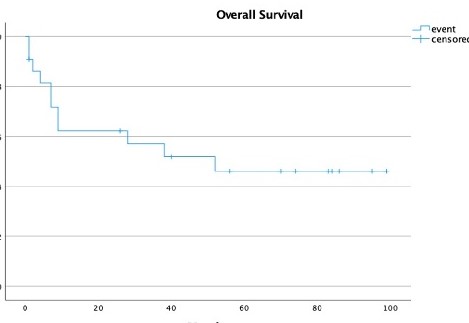
at 24 months 60% of patients were alive and in complete remission, median overall survival was not reached (figure 1). No septic death before engraftment or primary graft failure were noted. Only 1 patient never had platelets engraftment and subsequently developed secondary graft failure four months after HSCT. Median time to neutrophils ³ 1000/mL was 13 days (11-56), and 19 days (12-161) to platelets ³ 20.000/mL. Median CD3 and CD15 chimerism at day 100 were 97% and 99%, respectively. Overall incidence of acute GVHD was 54% (grade I-II 50%, grade III-IV 50%); chronic GVHD rate was 31% (mild 57%, moderate 28%, severe 15%). CMV reactivation occurred in 40% of patients, at a median of 50 days after transplant (29 - 165). Incidence of venous occlusive disease (VOD) was 13%. Overall, 11 patients died (50%); cause of death were GVHD (3), PTLD (1), sepsis (2), VOD (1), donor derived acute myeloid leukaemia (1), relapse (1), unknown (1).
Conclusion
In this retrospective study we demonstrated a good OS for high-risk MF. The use of MA conditioning and PBSC allowed a fast engraftment. Despite the small population, few cases of VOD were recorded as expected. The use of single agent ciclosporin as GVHD prophylaxis was not enough to avoid high rate of GVHD despite the use of in vivo T-cell depletion with ATG. In conclusion, MA HSCT seems a promising and safe curative option for high-risk MF in patients older than 55 years, but more strategies are needed to optimise the GVHD prophylaxis without increasing the rate of opportunistic infection or relapse.
Keyword(s): Cyclosporin A, Graft-versus-host disease (GVHD), Myelofibrosis
Abstract: EP1279
Type: E-Poster Presentation
Session title: Stem cell transplantation - Clinical
Background
The expected median survival of intermediate risk and high-risk myelofibrosis (MF) defined by dynamic international prognostic staging system (DIPSS) is of 2.9 and 1.3 years, respectively.
For that reason, allogeneic hematopoietic stem cell transplant (HSCT) is still considered the only curative option for those patients that are eligible for it.
The use of peripheral blood stem cell (PBSC) as graft source is allowing a fast engraftment, but there is still uncertainty among different centres about the most appropriate conditioning regimen in MF and the maximum age limit for myeloablative (MA) conditioning.
Aims
Herein we report the outcome of myeloablative HSCT in patients older than55 with high-risk MF as defined by DIPSS.
Methods
Between April 2012 and December 2018, 22 patients (10 high risk, 12 intermediate-2) with a median age of 61 (range 44-68 years) had full matched allogeneic stem cell transplant. HSCT was performed with GCSF mobilised PBSC. Conditioning protocol was with fludarabine 15 mg/m2 days -9, -8, -7, -6, -5, busulfan 3.2 mg/Kg days -6, -5, -4, -3; graft versus host disease (GVHD) prophylaxis consisted of thymoglobulin before transplant (ATG 5.5 mg/Kg until January 2015; ATG 5 mg/Kg since March 2016) and single agent ciclosporin 1.5 mg/Kg (therapeutic level of 200) until d+90 and then tapered. A median of 5x106 CD34+/Kg was infused (3.2 – 6). Donors were: 10 siblings, 11 unrelated donor, 1 mismatched unrelated donor.
Results
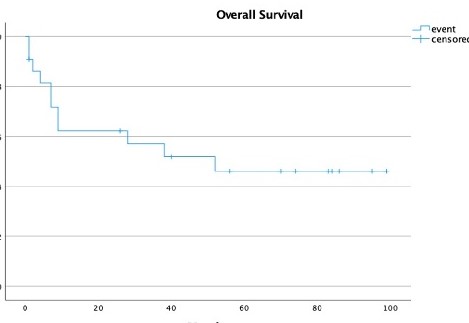
at 24 months 60% of patients were alive and in complete remission, median overall survival was not reached (figure 1). No septic death before engraftment or primary graft failure were noted. Only 1 patient never had platelets engraftment and subsequently developed secondary graft failure four months after HSCT. Median time to neutrophils ³ 1000/mL was 13 days (11-56), and 19 days (12-161) to platelets ³ 20.000/mL. Median CD3 and CD15 chimerism at day 100 were 97% and 99%, respectively. Overall incidence of acute GVHD was 54% (grade I-II 50%, grade III-IV 50%); chronic GVHD rate was 31% (mild 57%, moderate 28%, severe 15%). CMV reactivation occurred in 40% of patients, at a median of 50 days after transplant (29 - 165). Incidence of venous occlusive disease (VOD) was 13%. Overall, 11 patients died (50%); cause of death were GVHD (3), PTLD (1), sepsis (2), VOD (1), donor derived acute myeloid leukaemia (1), relapse (1), unknown (1).
Conclusion
In this retrospective study we demonstrated a good OS for high-risk MF. The use of MA conditioning and PBSC allowed a fast engraftment. Despite the small population, few cases of VOD were recorded as expected. The use of single agent ciclosporin as GVHD prophylaxis was not enough to avoid high rate of GVHD despite the use of in vivo T-cell depletion with ATG. In conclusion, MA HSCT seems a promising and safe curative option for high-risk MF in patients older than 55 years, but more strategies are needed to optimise the GVHD prophylaxis without increasing the rate of opportunistic infection or relapse.
Keyword(s): Cyclosporin A, Graft-versus-host disease (GVHD), Myelofibrosis


